
Samueli Institute Integrative Health Learning Collaborative Case
The Integrative Health Learning Collaborative sought to improve the delivery of whole-person care and make integrative health routine and regular in primary care. During the learning collaborative, the Susan Samueli Integrative Health Institute at the University of California, Irvine developed and piloted a process for inter-professional collaboration with providers who aren’t trained in integrative health, and re-affirmed the importance of integrative health and how institute leaders can support practice transformation at other clinics.
Introduction
The Burden of Chronic Disease
Six in 10 adults in the U.S. have at least one chronic disease, and four in 10 have two or more, according to the CDC.1 People in underserved communities bear far more of the burden of chronic disease than people in more affluent communities.
The COVID-19 pandemic emphasized these health and health care disparities. More people in underserved communities, especially those from racial and ethnic minority groups, got sick or dyed or were at higher risk of getting sick and dying from COVID-19 compared to the general population.
Even before the pandemic, primary care providers struggled to find the time, tools and resources to help patients with chronic diseases—whether affluent or underserved—improve their health and wellbeing. Yet, most chronic diseases seen in primary care can be prevented, managed or even reversed by addressing their underlying social and behavioral determinants.
A Better Way to Manage Chronic Disease
Whole-person care and integrative health focus on helping patients achieve health and wellbeing, not just on the treatment of disease, illness and injury. It is a better way to manage chronic disease because it addresses all the factors that impact health and healing:
- Medical treatment
- Mental health
- Personal behaviors and lifestyle
- Social determinants of health
- Personal determinants of healing
Integrative primary care providers use all proven approaches:
- Evidence-based conventional medicine
- Non-drug treatments (including complementary and alternative medicine)
- Self-care
They focus on what matters most to each person and establish trusting, ongoing relationships to help patients heal.
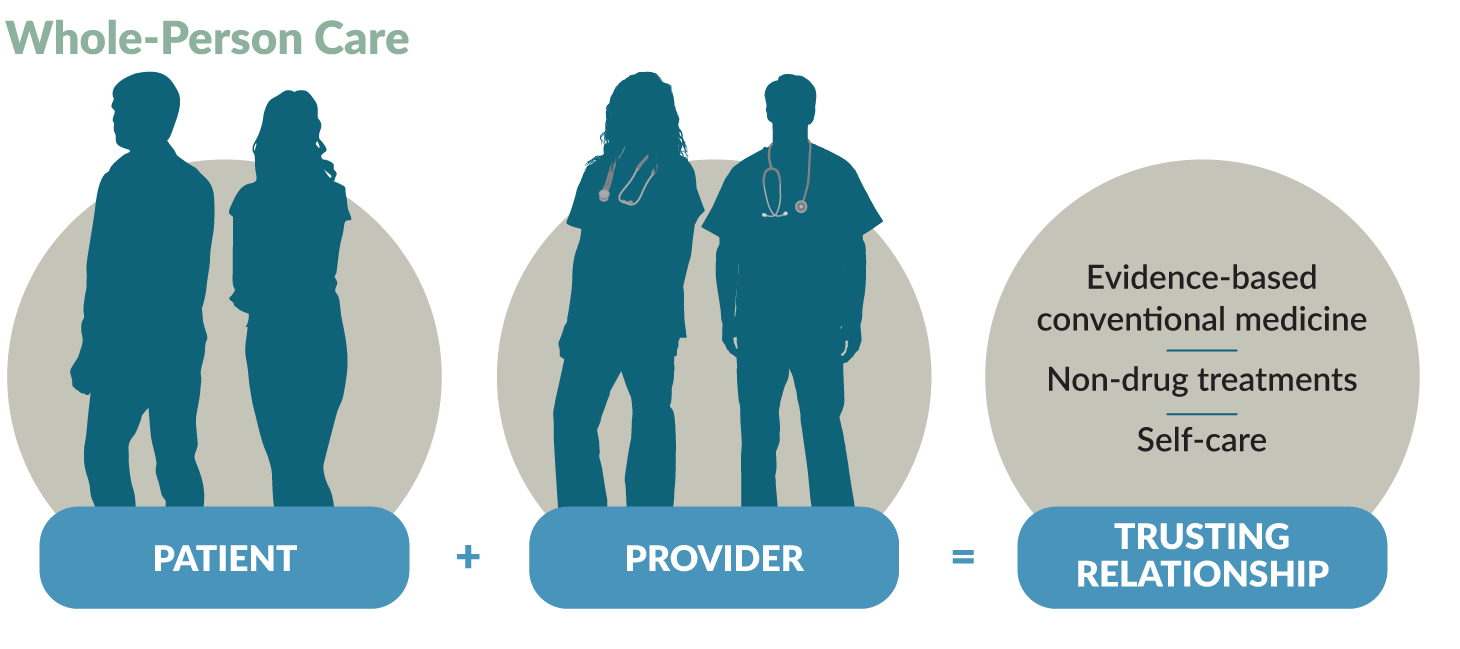
Whole-Person Care
Helps patients achieve health and wellbeing:
Integrative primary care providers use a person-centered, relationship-based approach to integrate self-care with evidence-based conventional medicine and non-drug treatments. They consider all factors that influence healing:
- Medical treatment
- Mental health
- Personal behaviors and lifestyle
- Social determinants of health
- Personal determinants of healing
Uses proven approaches:
Integrative primary care providers coordinate the delivery of evidence-based conventional medicine and non-drug treatments and self-care:
- Conventional medicine is the delivery of evidence-based approaches for disease prevention and treatment currently taught, delivered and paid for by the mainstream health care system.
- Non-drug treatments focus on non-pharmacological approaches to care and include what is sometimes called complementary and alternative medicine (CAM).
- Self-care is all the evidence-based approaches that individuals can engage in to care for their own health and wellbeing. Self-care promotes healthy behaviors and a healthy lifestyle to enhance health and healing. Approaches focus on the connection between the body, the mind the spirit and behavior, and cover food, movement, sleep, stress, substance use and more. Improving one area can influence the others and benefit overall health.
Goes beyond the doctor’s office to consider context:
Whole-person care is framed by each person’s social and personal context:
- Social determinants of health are the conditions in the places where people live, learn, work and play that affect health and quality of life.
- Personal determinants of healing are those personal factors which influence and promote health and healing. These include the physical, environmental, lifestyle, social, emotional, mental and spiritual dimensions which are connected and must be balanced for a happy and fulfilled life.
- Health Coaching is a delivery method for whole-person care. Health coaches use their expertise in human behavior to help individuals set and achieve health goals. They are an increasingly important component of whole-person care teams.
Providers work with patients to create a personalized health plan based on the person’s needs and preferences. To do this, they use free tools such as:
- The PHI (Personal Health Inventory), which assesses the person’s meaning and purpose in life, current health and readiness for change. Patients complete this before or during a primary care visit that integrates health and wellbeing.
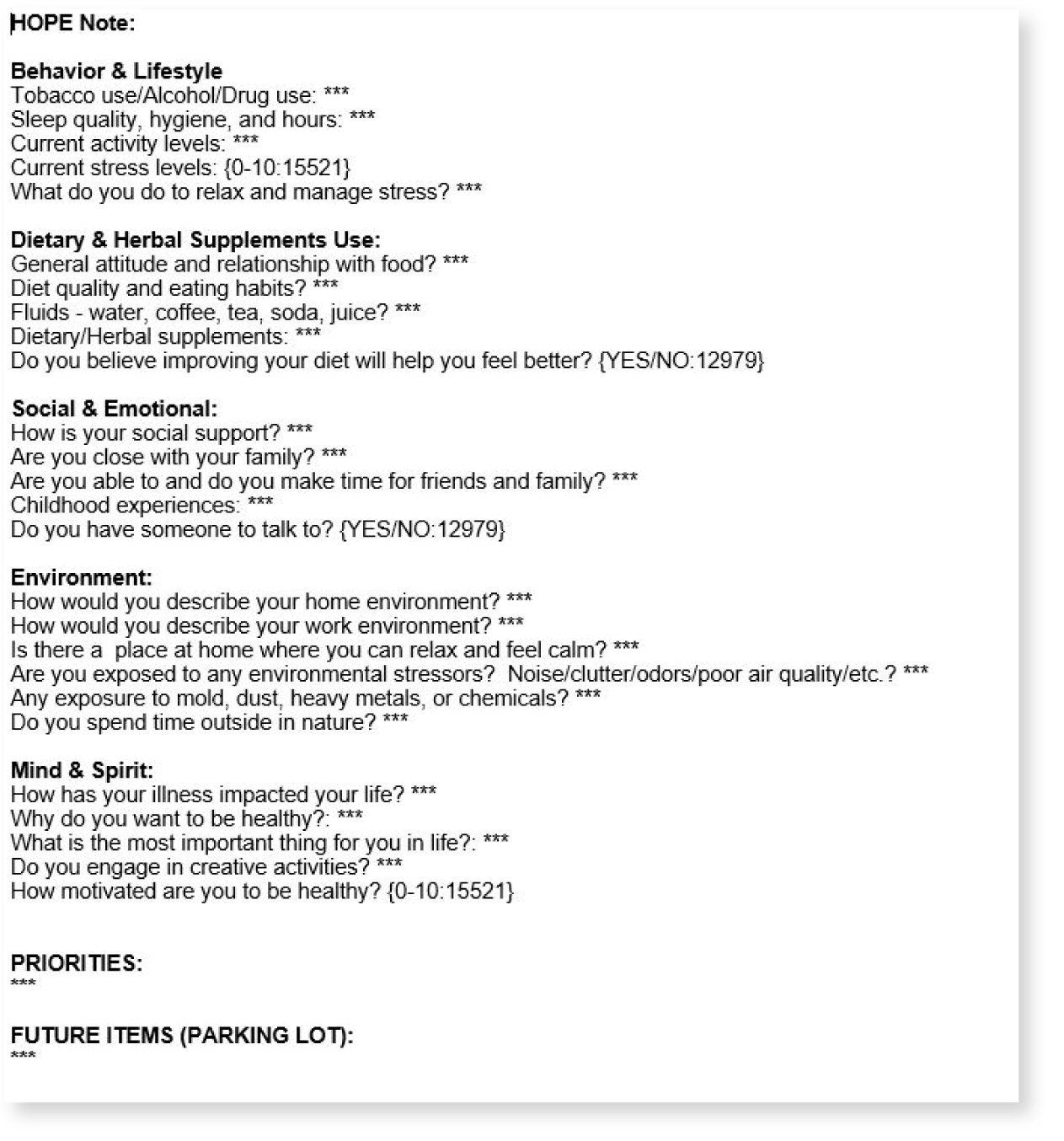
- The HOPE (Healing Oriented Practices & Environments) Note, a patient-guided process to identify the person’s values and goals in life and for healing so the provider can assist them in meeting those goals with evidence and other support.
Whole-Person Care Works
Evidence shows that whole-person care is effective in meeting the quadruple aim of:
- Better outcomes
- Improved patient experience
- Lower costs
- Improved clinician experience
Read more about the evidence supporting whole-person care.
The Integrative Health Learning Collaborative
The Integrative Health Learning Collaborative sought to better manage chronic disease by addressing social and behavioral determinants of health to:
- Improve the delivery of whole-person care
- Make integrative health routine and regular in primary care
Seventeen clinics participated in the learning collaborative, held from October 2020 to September 2021. The Family Medicine Education Consortium and Samueli Integrative Health Programs sponsored the learning collaborative, which was funded by a grant from The Samueli Foundation.
Read more about the Integrative Health Learning Collaborative.
An Evidence-Based, Integrative Approach to Health and Wellness
UCI Health, the clinical enterprise of the University of California Irvine (UC Irvine), is home to the Susan Samueli Integrative Health Institute. The only academic health system in Orange County California, UCI Health is a 459-bed acute care hospital providing tertiary and quaternary care, and ambulatory and specialty medical, behavioral health and rehabilitation services. It is the primary teaching location for UCI School of Medicine. In fiscal year 2021, UCI Health had more than one million outpatient visits, more than 28,000 patient discharges, more than 50,000 emergency department visits and more than 20,000 surgeries.
The Susan Samueli Integrative Health Institute helps patients achieve optimal health through an interdisciplinary, evidenced-based, integrative approach to health and wellness. Established in 2001, the institute focuses on preventing health problems such as chronic diseases instead of reacting to disease, illness and injury. UC Irvine also is embedding whole-person care into teaching and research across all four of its health sciences schools: medical, nursing, pharmacy and public health.
Providers at the Susan Samueli Integrative Health Institute use a patient-centered, whole-person, systems based and integrative approach to assess the many factors that impact health. Working closely with each patient, they tailor the treatments and therapies to each patient’s needs and circumstances.
The integrative health team includes:
- Integrative primary care and specialty physicians
- Naturopathic doctors
- Osteopathic physicians
- Nurse practitioners
- Psychologists
- Massage therapists
- Licensed acupuncturists
- Registered dietitians
Inter-professional collaboration among team members is strong. “We all share the same medical philosophy: whole-person care. We use different tools and modalities but we have mutual respect for what each provider can offer the patient,” says Jacob C. Hwang, ND, a naturopathic doctor at the Susan Samueli Integrative Health Institute.
Services include:
- Acupuncture
- Classes in:
- Mindfulness
- Tai chi
- Yoga
- Patient education
- Children’s health
- Executive health
- Group medical visits
- Integrative behavioral health
- Integrative biofeedback
- Integrative breast wellness program
- Integrative cardiology
- Integrative dermatology
- Integrative gastroenterology
- Integrative nutritional counseling
- Integrative pain management
- Integrative physical therapy
- Integrative weight management
- Massage therapy
- Naturopathic medicine
- Women’s health
- Yoga therapy
Team members also conduct rigorous research and educate medical students, residents and health care professionals.
Learn more about the Susan Samueli Integrative Health Institute.
Work During the Integrative Health Learning Collaborative
Expanding Integrative Health Through Communication and Collaboration
As a well-established integrative health clinic, the Susan Samueli Integrative Health Institute was already addressing social and behavioral determinants of health in primary care and helping patients achieve health and wellbeing. Leaders wanted to expand integrative practice into other clinics and specialties at UC Irvine.
While providers at the Susan Samueli Integrative Health Institute weren’t using the PHI or the HOPE Note before the Integrative Health Learning Collaborative, they were using similar concepts and elements to tailor treatments and therapies to each patient’s needs and circumstances. During the learning collaborative, they began using the HOPE Note and the PHI to expand opportunities for collaboration by teaching other providers how to do whole-person care even if they were not at the institute.
“Often, clinicians become siloed and communication and collaboration are lacking. We needed to improve communication and collaboration to provide truly whole-person and patient-centered care,” says Arvin Jenab, ND, medical director of Naturopathic Medicine and director of the ND Residency Program at UC Irvine and a naturopathic doctor at the Susan Samueli Integrative Health Institute
“Communication and collaboration are the first step in practice transformation.”
Dr. Jenab and his team wanted to start by collaborating with providers who were interested in bringing integrative health to their patients but didn’t have any training in it. As part of an academic medical center, the Susan Samueli Integrative Health Institute was already focused on teaching and systems change. Dr. Jenab and his team needed to figure out the best way for communicating and collaborating with these providers.
Also, as a national leader in integrative health, the team wanted to support other clinics that were implementing integrative health to help meet the Susan Samueli Integrative Health Institute’s mission of transforming health care through the practice of integrative health.
The Integrative Health Learning Collaborative Team
The team for the Integrative Health Learning Collaborative was led by Drs. Jenab and Hwang along with:
- Bavani Nadeswaran, MD, clinical professor of medicine
- Ashwini Erande, MPH, MSc, research associate
- Maryann Pack, chief administrative officer
Dr. Jenab oversaw the project, brought the team members together, and produced a clinical flowchart of the work. Dr. Hwang helped develop the HOPE Note template for the project, handled logistics, coordinated with other team members and tracked progress.
Dr. Nadeswaran, an internal medicine physician who specializes in primary care and bariatric medicine, served as the pilot for the learning collaborative project to expand interprofessional collaboration between integrative health providers and conventional medical providers.
Erande, the research associate for the Susan Samueli Integrative Health Institute, helped the team determine which validated questionnaires to use in addition to the PHI (PROMIS 10, SF-10 and PSS-10). Pack handled clinic logistics and compliance with the regulations.
In order to be able to accurately measure use of the HOPE Note in communicating and collaborating with conventionally-trained providers, the integrative health team focused on a provider with interest but no training in integrative health, Dr. Nadeswaran, and patients who were new to integrative health. Dr. Hwang created a provider training manual to aid Dr. Nadeswaran, provided one-on-one assistance to her and tracked her progress. The goal was to incorporate the process into a conventional provider’s workflow.
Patient Case: Integrative Health Helps Relieve GI Problems, ADHD, Anxiety and Stress
When Lisa (not her real name) went to see Dr. Nadeswaran, she was seeking relief from abdominal pain and bloating, tinnitus and a temporomandibular joint (TMJ) disorder. The 25-year-old had recently developed acute abdominal pain, which she rated as severe (8 out of 10, with 10 being the highest pain), and nausea. Lisa has had abdominal bloating since she was a teenager. She also reported constipation. Excedrin relieves Lisa’s migraines, but she has tinnitus during the migraines. Both tinnitus and TMJ disorder made it difficult for Lisa to sleep.
Dr. Nadeswaran referred Lisa to an acupuncturist, an integrative nutritional counselor, an integrative neuropsychologist, two naturopathic doctors and an integrative gastroenterologist. Acupuncture is reducing the severity and frequency of Lisa’s pain and has reduced her gastrointestinal symptoms. The integrative nutritional counselor gave Lisa dietary recommendations.
Currently, Lisa is receiving biofeedback treatment and psychotherapy from the integrative neuropsychologist for ADHD, anxiety and stress, diagnosed during her HOPE visit with Dr. Nadeswaran and visits with her naturopathic doctors. These treatments have improved Lisa’s mood and emotional control.
Lisa has seen two naturopathic doctors, one for integrative health management and one for integrative biofeedback. The naturopathic doctor involved in managing her overall integrative health focused primarily on addressing the gastrointestinal ailments and made an internal referral to the second
naturopathic doctor for integrative biofeedback treatment.
The second naturopathic doctor recommended nutraceuticals and supplements containing botanical extracts to support gastrointestinal function. Lisa will continue to receive acupuncture and see both naturopathic doctors on an as-needed basis.
Evaluating Whole-Person Care
The Susan Samueli Integrative Health Institute evaluated its use of integrative health for practice and clinical improvement. They used the Plan-Do-Study-Act (PDSA) cycle and the McKinsey 7S model of change management to plan and manage implementation and to evaluate their changes and plan next
steps to expand the delivery of integrative health.
Read more about PDSA cycles and the McKinsey 7S model of change management.
Here is what the Susan Samueli Integrative Health Institute did.
Key Results
Catalyzing Inter-Professional Collaboration
Clinic Highlights
The Susan Samueli Integrative Health Institute reported the following accomplishments related to work during the Integrative Health Learning Collaborative.
The integrative health team developed and piloted a process for inter-professional collaboration with providers who aren’t trained in integrative health.
The process included a clinical flowchart designed to introduce integrative health without significantly disrupting the usual workflow, use of the PHI and the HOPE Note and a training manual. The team piloted the process with Dr. Nadeswaran. As of September 2021, she had:
• Seen 12 patients who were new to integrative health
• Completed 13 PHIs and 19 HOPE visits
• Made 18 referrals for integrative health services.
“I like the integrative approach of whole-person care, instead of investigating symptoms, abnormal physical findings or abnormal labs…This kind of visit not only helps me to truly understand the patient but also to provide more personalized care.”
— Bavani Nadeswaran, MD
Dr. Nadeswaran liked having more time in an integrative health visit “to connect with the patient at a deeper level” and to learn more about the patient’s life, including diet, environment, support system, stressors and what makes the patient happy.
The clinical flowchart showed the steps in the process, from recruiting the patient to the initial consult, making referrals and collaborating with a naturopathic doctor or an integrative health specialist.
Clinical flowchart for collaboration between conventional and integrative health providers
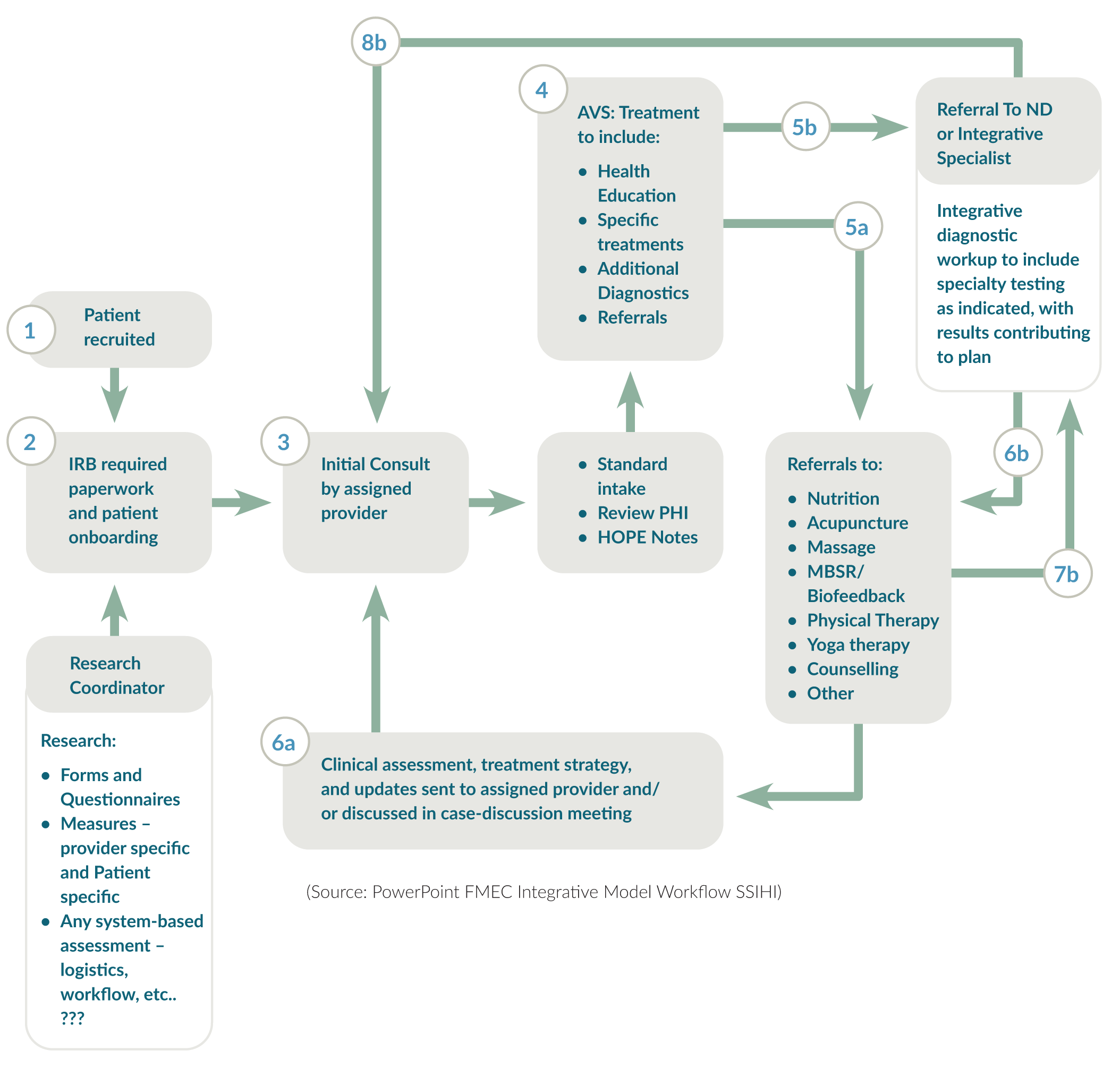
Patients fill out the PHI In the waiting room or the examination room before seeing the provider, who does the HOPE visit in a single visit.
“The HOPE Note was a nice introduction for Dr. Nadeswaran to think about what else she could consider rather than just drug therapy,” says Hwang. “It allowed for more collaborative treatment and further conversations and collaboration about integrative health.”
The training manual explains the PHI, the HOPE Note, integrative health visits, available integrative health services and resources and how to refer patients for services.
As a tool, the HOPE Note has many benefits for clinics, providers with little or no integrative health training and patients.
The HOPE Note can:
- Help providers solicit information from patients to help identify the social and behavioral determinants of health
- Be used to train providers with little or no training in integrative health to identify patients who can benefit from a team-based, holistic and comprehensive approach to health care
- Increase opportunities for team-based care by helping providers and the clinic identify resources to offer patients, including referrals, community resources and courses to address patients’ needs
- Catalyze collaboration by allowing providers and clinics to collaborate in delivering truly patient centered, whole-person care
Using the tool and the process to practice integrative health is challenging for traditional providers, says Dr. Jenab. Patients are complex and it can be overwhelming for experienced providers who are used to their own clinical workflow.
Instead, Dr. Jenab suggests using the HOPE Note with family medicine residents to help them understand integrative health. “If this will benefit medicine, it needs to be designed and targeted to family medicine residents, who will start to think about these things in their formative years,” he says.
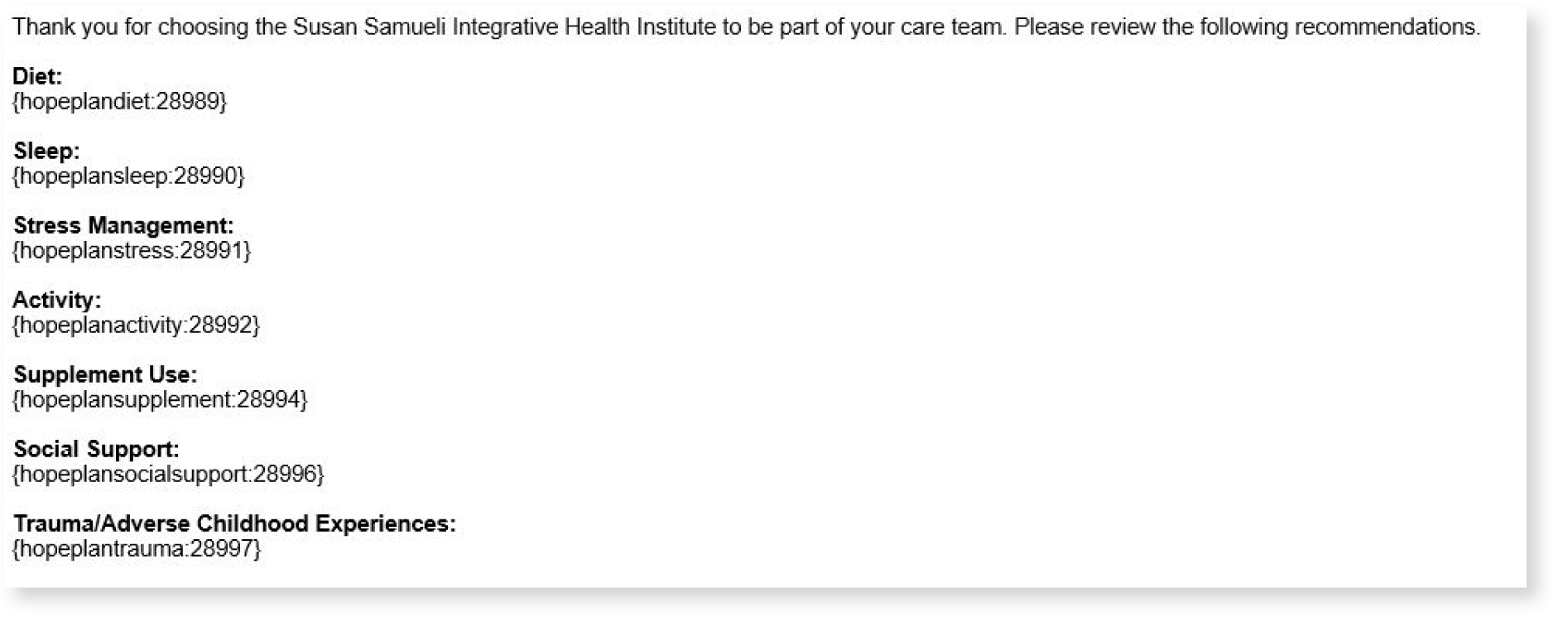
Incorporating the HOPE Note into an EMR facilitates integrative health.
The integrative health team developed a HOPE Note template and plan into Epic using a SmartPhrase. This enables non-integrative health providers to easily pull a patient’s chart and summary, become familiar with integrative health services and add notes. Over time, the team will adjust and improve the SmartPhrase, and may eventually develop a SmartSet.
Also, Dr. Hwang used Epic to track Dr. Nadeswaran’s integrative health work, along with an Excel spreadsheet with data from the PHI and other questionnaires.
HOPE Note template in Epic
HOPE Note plan in Epic
Learning Collaborative Highlights
The Susan Samueli Integrative Health Institute reported the following benefits of participating in the Integrative Health Learning Collaborative.
Meeting and collaborating with other clinics interested in integrative health confirmed the importance of integrative health and the work of the Susan Samueli Integrative Health Institute.
Conversations with colleagues across multiple clinics reaffirmed the importance of integrative health and the work of the Susan Samueli Integrative Health Institute.
The Integrative Health Learning Collaborative highlighted the need for experts such as those at the Susan Samueli Integrative Health Institute to support practice transformation.
Clinics participating in the learning collaborative want to provide more integrative care. “They’re hungry for a solution to some of the challenges they’re facing,” says Dr. Jenab.
During the learning collaborative, the integrative health team at the Susan Samueli Integrative Health Institute shared their expertise, including how they met challenges in developing their program, with the other clinics.
“We can’t expect the system to change without a structure or blueprint that supports change,” says Dr. Jenab. “We have the means and the opportunity to support practice transformation. Participating in the Integrative Health Learning Collaborative highlighted our responsibility to do this.”
Collaborating with the Family Medicine Education Consortium was a great opportunity to help transform health care.
“It was exciting to be part of the conversation to transform health care,” says Dr. Hwang. He also found the small group discussions, led by a faculty member experienced in integrative health, useful and “a safe space to bounce off ideas.”
Key Insights for Implementing Integrative Health
Build inter-professional collaboration. Integrative health requires conventional and integrative health providers to collaborate and communicate. Mutual respect and a shared philosophy of providing wholeperson care facilitate the delivery of integrative health. When treating patients of conventional providers, communicate, share the assessment of the patient, focus on enhancing patient care and use evidence. Providers want to understand the rationale for the treatment their patients receive, especially if it is outside mainstream medicine. It is important to emphasize that integrative health is designed to enhance, not undermine, the care of other providers. The Susan Samueli Integrative Health Institute also provides references to show the science and research behind integrative health..
When introducing conventional providers to integrative health, provide training on whole-person care. Providers who are new to integrative health need more than an introduction to the PHI and HOPE Note to practice integrative health. Dr. Jenab suggested developing a training workshop, possibly for CME credits, on how to practice whole health. Dr. Nadeswaran also notes that providers who are interested in integrative health can learn on their own about integrative therapies for chronic diseases and resources that are available to their patients.
Use lunch and learn meetings to facilitate learning and collaboration and communication with conventional providers. The Susan Samueli Integrative Health Institute finds that lunch and learn meetings are a great way to teach conventional providers about integrative health and begin to build inter-professional collaboration. Conventional providers feel comfortable asking questions during these informal meetings.
Train family medicine residents in integrative health. It is much easier for family medicine residents to learn about and practice integrative health than conventional providers who have been practicing for many years. Departments of family medicine should play a key role in training family medicine residents in integrative health.
A SmartPhrase is an easy way to start incorporating the HOPE Note into an EMR. The integrative health team at the Susan Samueli Integrative Health Institute was able to develop the SmartPhrase on its own, whereas developing a SmartSet would have required bringing in the Epic build team. This
would have taken months. A SmartSet, however, is a better tool that can direct the provider in making choices. Also, diagnostic codes, patient handouts and referrals can be built into a SmartSet.
Challenge
Integrative Health is Complex
Introducing integrative health to conventional providers is complex. The modified HOPE Note tool and process developed and used during the Integrative Heath Learning Collaborative wasn’t sufficient for a conventional provider to learn how to practice integrative health fully. Dr. Nadeswaran found it difficult to navigate the integrative health referral options due to limited knowledge and experience working with integrative health professionals.
The integrative health team gave her more autonomy to modify the HOPE Note and to set a time limit for completion of paperwork by patients. Dr. Jenab suggests developing a readiness scale to see if providers and teams are ready to use the HOPE Note and training them on whole-person care.
Next Steps
Continuing to Build Inter-Professional Collaboration
The Susan Samueli Integrative Health Institute plans to continue to increase inter-professional collaboration between integrative and conventional providers. The team will refine the HOPE Note tool and process developed during the Integrative Health Learning Collaborative and explore the most effective ways to use them to communicate and collaborate with conventional providers to provide patients with patient-centered, whole-person care.
Appendix 1
Evidence from existing whole-person care supports the effectiveness of this model in meeting the quadruple aim:
- Better Outcomes
- Improved Patient Experience
- Lower Costs
- Improved Clinician Experience.
This evidence includes a narrative review of several models of whole-person care and studies illustrate the business case for whole-person models in primary care2 and the models and studies cited in this section.
Better Outcomes
Whole-person care:
- Increases the ability to manage chronic pain and decreases opioid doses.3
- Improves patient-reported health and wellbeing.4
- Lowers A1c in people with diabetes.5
- Improves medication adherence.6
- Facilitates a healthier lifestyle.7
- Reduces the severity of heart disease.8, 9
- Reduces loneliness among seniors.10
- Lessens symptoms, including pain, depression, low back pain and headaches.11, 12, 13
Improved Patient Experience
Whole-person care:
Lower Costs
Improved Clinician Experience
Appendix 2
PDSA Cycles and the McKinsey 7S Model of Change Management
The PDSA Cycle
The PDSA cycle is a tool for documenting change. Clinics participating in the Integrative Health Learning Collaborative planned and tested small changes, learned from the results, and modified the changes as necessary.
PDSA Cycle
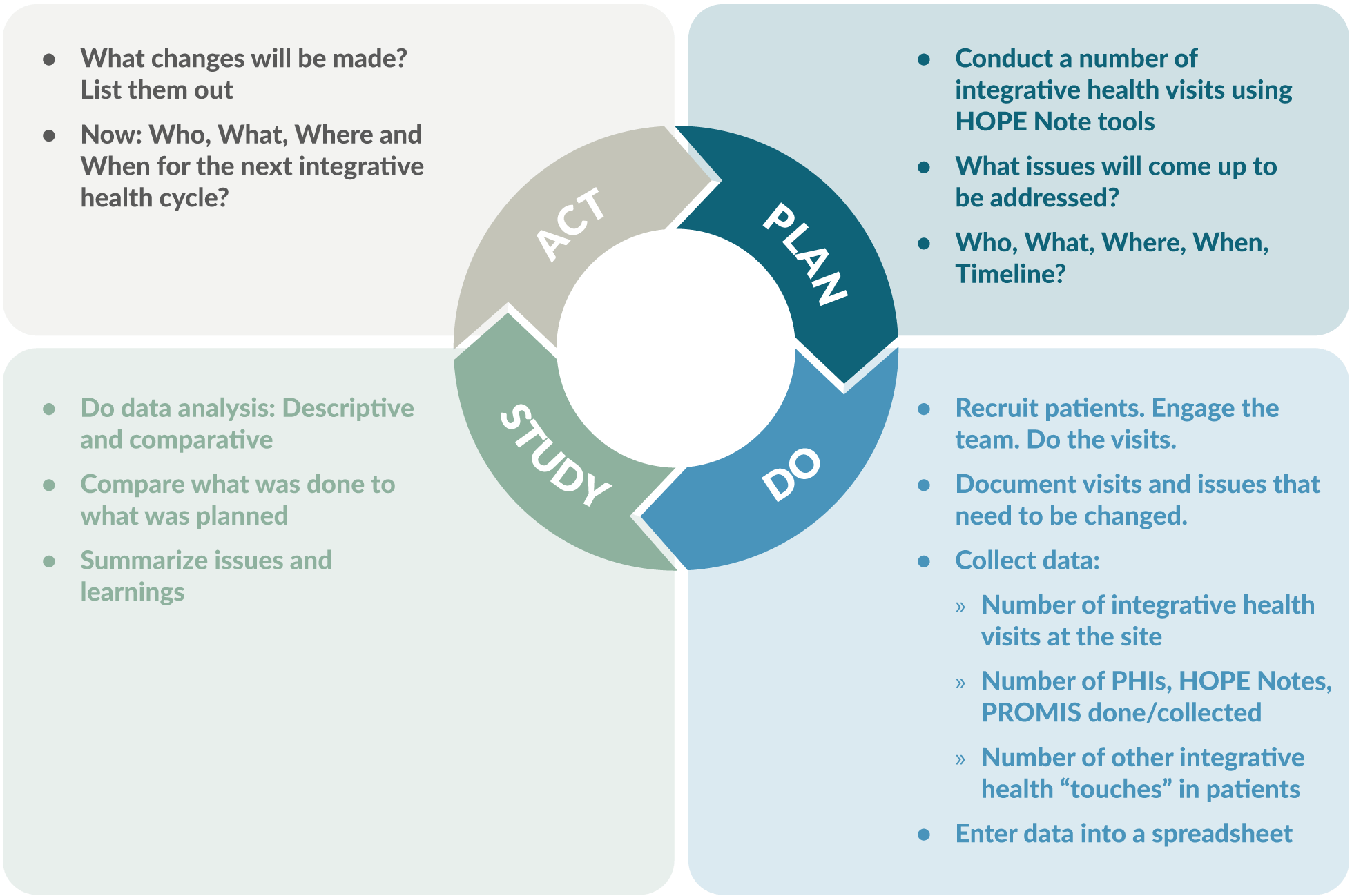
Source: Slide 9, PDSA and 7S Report Outs v1
The McKinsey 7S Model of Change Management
The McKinsey 7S model of change management is a good way to plan and manage implementation of integrative health. The model considers three structural elements: strategy, systems and structure. It also recognizes three “people” elements needed to win the hearts of everyone from front office staff
to the most senior physicians. These include addressing the types of people who are going to lead the change, the skills of the people who will be involved, and the overarching leadership style within the organization. These elements are fuzzier, more intangible, are influenced by corporate culture and are sometimes more difficult to address.
The McKinsey 7S Model of Change Management
Graphic CC-BY 2.5 Wikimedia
Managing change by addressing all these barriers leads to the 7th “S,” creation of shared values underpinning the culture of the group.
Structural and People Elements in the McKinsey 7S Model of Change Management
| Structural Elements: | |
|---|---|
| Strategy: | What do you want to do differently? What will it replace? |
| Systems: | What changes in workflow needs to happen to do the new thing? |
| Structure: | How are you going to set up a new system to kick off and then monitor the initiative? |
| People Elements: | |
| Style: | How are you going to lead the change? |
| Staff: | Who can you enlist who will make it happen? Who do others in your practice look to for guidance? |
| Skills: | Who needs to be trained in the new workflow? What is the training? How can you give them ownership? |
Addressing all these issues through careful planning will lead to development of the shared values, the commonly accepted standards and norms within the practice that will make the switch to whole-person care a success.
Using the 7S Model to Plan Implementation
Substantial planning is necessary to make the change to whole-person care.
Strategy: The obvious changes, as part of this initiative, are to start using the PHI, start conducting integrative visits around the HOPE note, and start setting up a way to monitor both your implementation and the outcomes you’ve settled on. Who is going to do what?
Systems: Careful attention is needed to identify new systems to support whole-person care. Most aspects of the practice will need to be changed in some way, including front-office, billing, and clinical care workflows. Having a Plan B on the shelf will be useful.
Structure: Determine how the roll-out will occur. It may be best to start a pilot project with a single team, carefully chosen for their ability to embrace change. Their success must be carefully monitored so that processes can change when barriers are discovered.
Style: Decide on whether the change to whole-person care will be incremental or dramatic. Decide on who will lead the implementation and how they will approach it. Develop a means of getting staff members excited. Decide how much input the staff will have in the implementation. Set up a rapid cycle quality improvement plan.
Staff: You will need to enlist key people to make your implementations happen and to make it stick. These may be people in key roles, but you will need to identify an opinion leader and a first follower (the first person in the organization to support the opinion leader) for the implementation to be widely adopted.
Skills: Whole-person care requires a new set of skills and new practices. Identify who will need to receive new training and determine how to provide the training.
The McKinsey model is probably well known to most hospital administrators but less known to clinicians and managers. Soon a five-part continuing medical education series for clinicians, staff and managers will be available that explains the HOPE note and introduces integrative health to the team and managing and monitoring the implementation process.
Endnotes
- Chronic Disease in America. https://www.cdc.gov/chronicdisease/tools/infographics.htm. Accessed 10/25/21.
- Jonas, W, Rosenbaum E. The Case for Whole-Person Integrative Care. Medicina. 30 June 2021. https://www.mdpi.com/1648-9144/57/7/677/htm. Accessed 11/8/21.
- Bokhour BG, Hyde J, Zeliadt S, Mohr H. Whole Health System of Care Evaluation – A Progress Report on Outcomes of the WHS Pilot at 18 Flagship Sites. February 18, 2020. Veterans Health Administration, Center for Evaluating Patient-Centered Care in VA (EPCC-VA). https://www.va.gov/WHOLEHEALTH/docs/EPCC_WHSevaluation_FinalReport_508.pdf. Accessed 7/15/21.
- Crocker R, Hurwitz JT, Grizzle AJ, et al. Real-World Evidence from the Integrative Medicine Primary Care Trial (IMPACT): Assessing Patient-Reported Outcomes at Baseline and 12-Month Follow-Up. Evidence-Based Complementary and Alternative Medicine, 2019, Article ID 8595409. https://doi.org/10.1155/2019/8595409. Accessed 7/15/21.
- Hojat M, Louis DZ, Markham FW, Wender R, Rabinowitz C, Gonnella JS. Physicians’ empathy and clinical outcomes for diabetic patients. AcadMed. 2011 Mar;86(3):359-64. doi: 10.1097/ ACM.0b013e3182086fe1. PMID: 21248604. https://journals.lww.com/academicmedicine/Fulltext/2011/03000/Physicians__Empathy_and_Clinical_Outcomes_for.26.aspx. Accessed 7/15/21.
- Zolnierek KB, Dimatteo MR. Physician communication and patient adherence to treatment: a meta-analysis. Med Care. 2009 Aug;47(8):826-34. doi: 10.1097/MLR.0b013e31819a5acc. PMID: 19584762; PMCID: PMC2728700. https://pubmed.ncbi.nlm.nih.gov/19584762/. Accessed 7/15/21.
- Budzowski AR, Parkinson MD, Silfee VJ. An Evaluation of Lifestyle Health Coaching Programs Using Trained Health Coaches and Evidence-Based Curricula at 6 Months Over 6 Years. Am J Health Promot. 2019 Jul;33(6):912-915. doi: 10.1177/0890117118824252. Epub 2019 Jan 22. https://pubmed.ncbi.nlm.nih.gov/30669850/. Accessed 7/15/21.
- Estruch R, Ros E, Salas-Salvadó J, at al. Primary Prevention of Cardiovascular Disease with a Mediterranean Diet Supplemented with Extra-Virgin Olive Oil or Nuts. N Engl J Med 2018; 378:e34. DOI: 10.1056/NEJMoa1800389. https://www.nejm.org/doi/full/10.1056/NEJMoa1800389. Accessed 7/15/21.
- Ornish D, Scherwitz LW, Billings JH, et al. Intensive Lifestyle Changes for Reversal of Coronary Heart Disease. JAMA, December 16, 1998—Vol 280, No. 23. https://pubmed.ncbi.nlm.nih.gov/9863851/. Abstract accessed 7/15/21.
- Thomas KS, Akobundu U, Dosa D. More Than A Meal? A Randomized Control Trial Comparing the Effects of Home-Delivered Meals Programs on Participants’ Feelings of Loneliness. J Gerontol B Psychol Sci Soc Sci. 2016 Nov;71(6):1049-1058. doi: 10.1093/geronb/gbv111. Epub 2015 Nov 26. PMID: 26613620. https://pubmed.ncbi.nlm.nih.gov/26613620/. Accessed 7/15/21.
- Huston P, McFarlane B. Health benefits of tai chi: What is the evidence? Can Fam Physician. 2016 Nov;62(11):881-890. PMID: 28661865. https://www.cfp.ca/content/62/11/881. Accessed 7/15/21.
- Department of Veterans Affairs. Evidence Map of Acupuncture. 2014. https://www.hsrd.research.va.gov/publications/esp/acupuncture.pdf. Accessed 7/15/21.
- Department of Veterans Affairs. Evidence Map of Mindfulness. 2014. https://www.hsrd.research.va.gov/publications/esp/cam_mindfulness-REPORT.pdf. Accessed 7/15/21.
- Press Ganey. Protecting Market Share in the Era of Reform: Understanding Patient Loyalty in the Medical Practice Segment. White Paper. 2013. http://img.en25.com/Web/PressGaneyAssociatesInc/PerfInsights_PatientLoyalty_Nov2013.pdf?elq=a66e16008286435885d97352358aefd3. Accessed 7/15/21.
- Crocker, R.L., Grizzle, A.J., Hurwitz, J.T. et al. Integrative medicine primary care: assessing the practice model through patients’ experiences. BMC Complement Altern Med 17, 490 (2017). https://doi.org/10.1186/s12906-017-1996-5. Accessed 3/10/21.
- The Impact of Relationship-Based Care. South Central Foundation Nuka System of Care. https://scfnuka.com/impact-relationship-based-care/. Accessed 3/10/21.
- Myklebust M, Pradhan EK, Gorenflo D. An integrative medicine patient care model and evaluation of its outcomes: the University of Michigan experience. J Altern Complement Med. 2008 Sep;14(7):821-6. doi: 10.1089/acm.2008.0154. PMID:18721082. https://deepblue.lib.umich.edu/bitstream/handle/2027.42/63379/acm.2008.0154.pdf;sequence=1 . Accessed 7/15/21.
- Cover Commission. Creating Options for Veterans’ Expedited Recovery: Final Report. January 24, 2020. https://www.va.gov/COVER/docs/COVER-Commission-Final-Report-2020-01-24.PDF. Accessed 7/15/21.
- Sarnat RL, Winterstein J. Clinical and cost outcomes of an integrative medicine IPA. Journal of Manipulative and Physiological Therapeutics. 2004 Jun;27(5):336-347. DOI: 10.1016/j.jmpt.2004.04.007. https://cdn.ymaws.com/nebraskachiropractic.org/resource/resmgr/Docs/Clinical_and_Cost_Outcomes.pdf. Accessed 7/15/21.
- Pruitt Z, Emechebe N, Quast T, Taylor P, Bryant K. Expenditure Reductions Associated with a Social Service Referral Program. Popul Health Manag. 2018 Dec;21(6):469-476. doi: 10.1089/pop.2017.0199. Epub 2018 Apr 17. PMID: 29664702; PMCID: PMC6276598. https://pubmed.ncbi.nlm.nih.gov/29664702/. Accessed 7/15/21.
- Jonk Y, Lawson K, O’Connor H, Riise KS, Eisenberg D, Dowd B, Kreitzer MJ. How effective is health coaching in reducing health services expenditures? Med Care. 2015 Feb;53(2):133-40. doi: 10.1097/ MLR.0000000000000287. PMID: 25588134. https://pubmed.ncbi.nlm.nih.gov/25588134/. Accessed 7/15/21.
- Cherkin DC, Herman PM. Cognitive and Mind-Body Therapies for Chronic Low Back Pain and Neck Pain: Effectiveness and Value. JAMA Intern Med. 2018;178(4):556–557. doi:10.1001/jamainternmed.2018.0113. https://jamanetwork.com/journals/jamainternalmedicine/articleabstract/2673371. Accessed 7/15/21.
- De Marchis E, Knox M, Hessler D, Willard-Grace R, Olayiwola JN, Peterson LE, Grumbach K, Gottlieb LM. Physician Burnout and Higher Clinic Capacity to Address Patients’ Social Needs. J Am Board Fam Med. 2019 Jan-Feb;32(1):69-78. doi: 10.3122/jabfm.2019.01.180104. PMID: 30610144. https://pubmed.ncbi.nlm.nih.gov/30610144/. Accessed 7/15/21.
- Wilkinson H, Whittington R, Perry L, Eames C. Examining the relationship between burnout and empathy in healthcare professionals: A systematic review. Burn Res. 2017 Sep;6:18-29. doi: 10.1016/j.burn.2017.06.003. PMID: 28868237; PMCID: PMC5534210. https://pubmed.ncbi.nlm.nih.gov/28868237/. Accessed 7/15/21.
- Eby D, Ross L. Internationally Heralded Approaches to Population Health Driven by Alaska Native/American Indian/Native American Communities. Institute for Healthcare Improvement 8th annual National Forum, 2016. http://app.ihi.org/FacultyDocuments/Events/Event-2760/Presentation-14234/Document-11589/Presentation_L2_Internationally_Heralded_Approaches_to_Population_Health_driven_by_Alaska_NativeAmerican_IndianNative_American_Communities_Eby.pdf. Accessed 7/15/21.
- Finnegan J. Integrative medicine physicians say quality of life is better. Fierce Healthcare. August 22, 2017. https://www.fiercehealthcare.com/practices/doctorspracticing-integrative-medicine-say-quality-life-better.Accessed 7/15/21.
Topics: Integrative Health
