
Case Study: Community Health System Frederick Health Makes Whole Person Cancer Care Routine
Cancer Care in a Community Health System
A Healing Environment for Patients, Family Members and Staff
Frederick Health is a not-for-profit health system in Frederick, Maryland, located about 50 miles northwest of Washington, DC, and 50 miles west of Baltimore. The system provides a full spectrum of health care and wellness services in Frederick County and includes the James M Stockman Cancer Institute.
The Role of Community Health Systems in Cancer Care
Community health systems like Frederick Health play a critical role in cancer care. They provide patients
located outside of metropolitan areas with convenient, affordable care and help meet the increasing
demand for cancer care.
“Frederick Health is just far enough away from Johns Hopkins Medicine in Baltimore and DC that there was a great need to have better cancer care locally,” says Wayne Jonas, MD, president of Healing Works Foundation and a clinical professor in the Department of Family Medicine at Georgetown University.
Approximately 85% of cancer patients in the United States receive care in community settings, not at academic medical centers. 1
Serving More Patients
Frederick Health wanted to be able to serve more patients with cancer, and they wanted to provide more holistic care. In 2015, they brought in Patrick Mansky, MD, as Medical Director of oncology and integrative services to do this. Dr. Mansky, a nationally recognized integrative oncologist, wanted to advance cancer care in a community setting. “We wanted to go beyond building four walls and giving cancer treatments to building a healing environment that benefits patients, their family members, and our staff,” he says.
A member of the National Cancer Institute’s PDQ editorial review board for PDQ® Cancer Information for Health Professionals, Dr. Mansky was the founding director of the Integrative Medicine Consult Service at the National Institutes of Health’s National Center for Complementary and Alternative Medicine (now called National Center for Complementary and Integrative Health) and the coordinator of the Complementary and Alternative Medicine Oncology Fellowship Program. In Germany, where Dr. Mansky completed medical school at University Witten/Herdecke, he studied anthroposophical medicine, an integrative medical system that is patient-centered, individualized, and holistic.
Promoting Healing and Alleviating Stress
Dr. Mansky wanted to promote healing and relieve anxiety by building an optimal healing environment for cancer care at the James M Stockman Cancer Institute at Frederick Health. Created by Samueli Institute in 2004, an optimal healing environment describes a health care system that is designed to stimulate and support the inherent healing capacity of patients, families, and their care providers. An optimal healing environment consists of people in relationships, their health-creating behaviors, and the surrounding physical environment.2
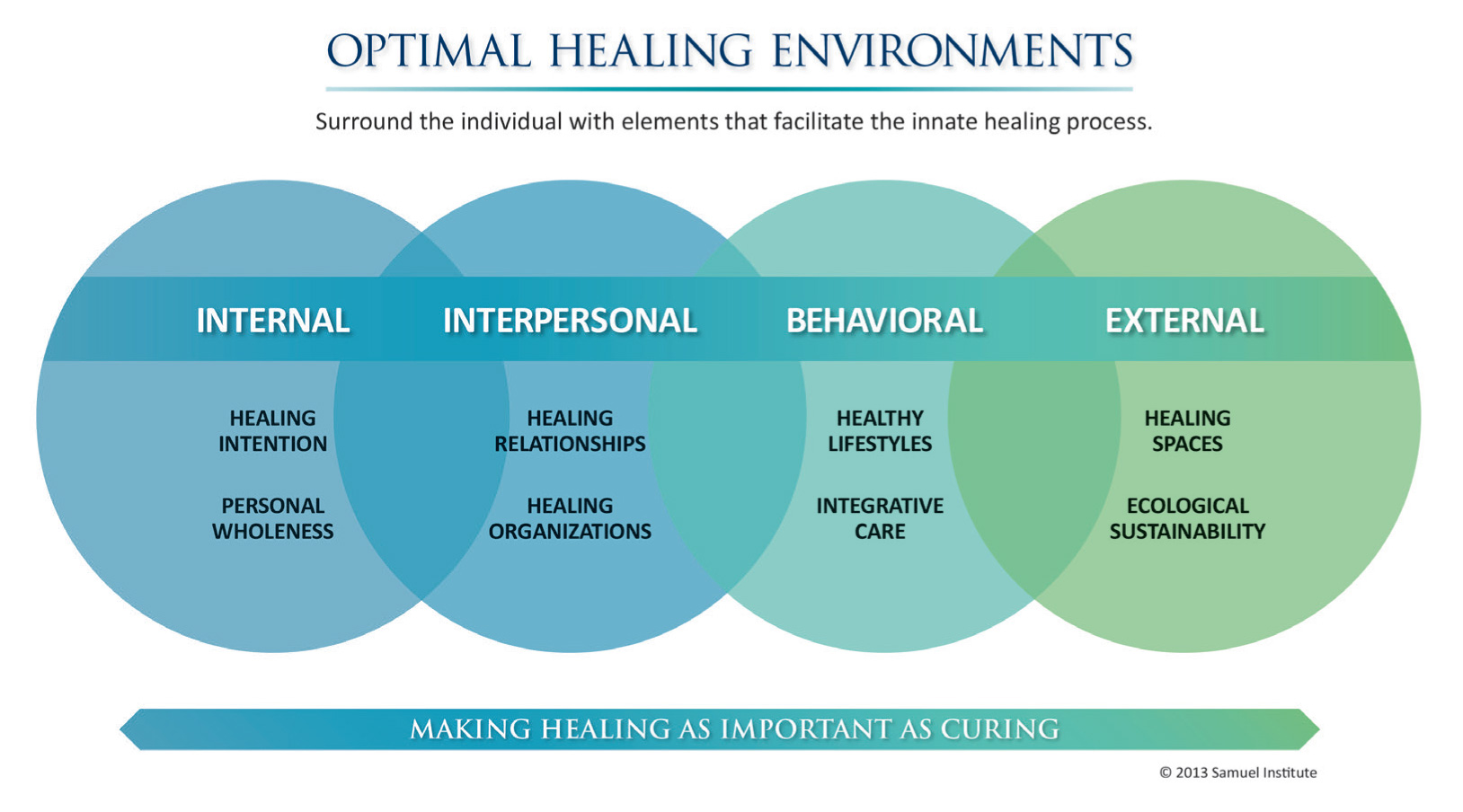
Components of an Optimal Healing Environment
- Conscious development of intention, awareness, expectation and belief in healing.
- Transformative self-care practices that facilitate personal cohesion and the experience of wholeness and well-being.
- Techniques that foster healing presence based on compassion, love, and awareness of interconnectivity.
- Development of listening and communication skills that foster trust and a bond between practitioner and patient.
- Instruction and practice in health promotion behaviors that change lifestyle to support self-healing and the development of social support.
- Responsible application of integrative medicine via collaborative practice supportive of healing processes.
- The physical space in which healing is practiced.
The Optimal Healing Environment at James M Stockman Cancer Institute
Samueli Institute consulted with Dr. Mansky to map out the process for and to train staff on an optimal healing environment. Together, they used this model in designing interior and exterior spaces, clinical workflows, and treatment planning at the James M Stockman Cancer Institute.
Physicians, clinicians, and staff are trained in the application of this model to promote healing and alleviate stress for patients during their cancer experience. Healing spaces within the institute’s external environment include:
- The color orange in public spaces to promote feelings of energy, along with natural textures and nature-based art.
- Green tones and views of the healing garden in the infusion center to evoke feelings of renewal.
- Inspiring, calming, natural images using yellow tones to inspire joy in the oncology and hematology patient areas.
The Integrative Services Program
Improving Patients' Outcomes and Quality of Life
Being diagnosed with cancer and going through treatment takes a toll on the body and the mind. While necessary, conventional standard of care treatments for tumor-directed therapy such as chemotherapy, radiation, or surgery may be quite demanding on the patient. These treatments and their side effects may significantly affect the quality of people’s lives.
“There’s more and more evidence that complementary therapies can be helpful for patients. They provide an additional opportunity for patients to receive optimal care.”
— Patrick Mansky, MD
After building the optimal healing environment at the James M Stockman Cancer Institute, Dr. Mansky wanted to add services to support and bolster patients’ tolerance for conventional cancer care and restore quality of life. He began to incorporate evidence-based integrative services into cancer care with a focus on complementary therapies.
Dr. Mansky also began to consider how to fund integrative cancer services through charitable contributions and subsidized payments from patients.
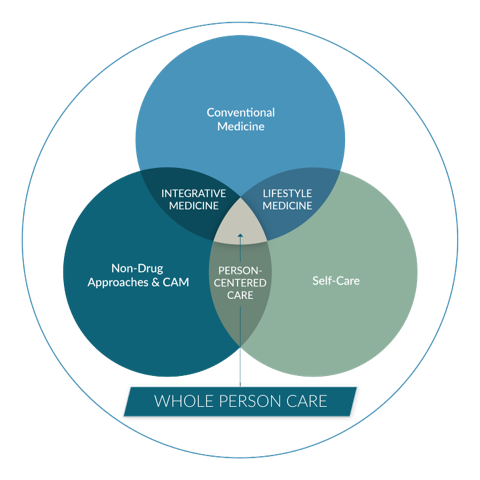
Using a Whole Person Approach to Cancer Care
Integrative services are part of a comprehensive whole person approach to cancer care. Whole person cancer care seeks to promote recovery and well-being while managing disease. The importance of “what matters” to the person guides treatment planning alongside “what’s the matter” (the disease). Managing issues with sleep, pain, anxiety, financial barriers, and sexual health that occur outside of the exam room, infusion center, or operating theater are part of what matters to patients.
Developing the Program
Dr. Mansky convened a stakeholder group to select the complementary therapies the James M Stockman Cancer Institute would provide. The group included cancer survivors, integrative service practitioners from the community, patient advocates, supporters of Frederick Health, and community members.
With a focus on complementary therapies with strong evidence supporting their use in cancer care, Dr. Mansky and the group chose four complementary therapies to offer:
- Acupuncture
- Massage
- Meditation
- Yoga
All services are offered on-site and delivered by professional practitioners with training and experience in working with cancer patients. The practitioners are independent contractors who live and work in the community.
Massage is an individual service while acupuncture, meditation, and yoga are available both as an individual service and in group sessions. Most patients take yoga and meditation classes. Acupuncture is primarily an individual service, but some group sessions are available.
Cancer survivor Claudia Olson, Mac Lic Ac, is one of the licensed acupuncturists who treats patients at the James M Stockman Cancer Institute. “I can’t image doing anything else,” she says.
Olson started the group acupuncture sessions for patients who had completed their active cancer treatment and were doing well but wanted to continue their acupuncture treatments. Each group has five or six patients. During the one-hour sessions, the participants share information and discuss their cancer journey, building a community that is similar to a support group.
Visit the James M Stockman Cancer Institute’s Integrative Services web page.
Funding Integrative Services
The James M Stockman Cancer Institute funds integrative services through charitable contributions and subsidized payments from patients. Philanthropy includes proceeds from pharmaceutical fairs, which the institute hosts quarterly.
“We do Pharmafairs instead of dinners or lunches. The pharmaceutical companies embrace and welcome this,” says Dr. Mansky.
Because charitable contributions do not cover all of the costs of integrative services, Frederick Health subsidizes the patients’ share of the cost. The intake visits include a financial screening and a description of the sliding fee scale for integrative services, which follow general Frederick Health practices and guidelines for financial assistance to patients.
In 2024, 55% of patients qualified for financial assistance. The highest co-pays for integrative services were $15 for a class and $65 for an individual service. Some patients qualify for no co-pay for these services.
Connecting Patients with Integrative Services
From the initial intake to recovery or supportive care, the cancer care team at the James M Stockman Cancer Institute continually assesses patient needs and develops personalized treatment plans for each person. Along with conventional treatments and integrative services, the plan includes:
- Nutrition and fitness support
- Nurse navigation across medical, surgical, and radiation domains
- Social work, including therapeutic counseling
- Financial counseling
- Palliative care, when necessary
“New patients have a comprehensive care visit, which includes meeting an oncologist and the support team (social workers, nurse navigators and financial counselors). As part of supportive care, we share information about our integrative services,” says Dr. Mansky. This information includes a discussion of available services and a binder with descriptions of these services.
The initial intake spans several visits. Nurse navigators and social workers assess patients for issues, such as pain, anxiety, and depression, that integrative services can relieve.
Jody Pritt, LCSW-C, OSW-C, APHSW-C, the integrative and support services coordinator and an oncology social worker and patient navigator, meets with each patient. She reviews the integrative services they’ve been referred to and discusses them with the patient.
During treatment, nurse navigators and social workers reassess patients and remind them about the available integrative services. Medical oncologists also recommend integrative services to help their patients manage symptoms such as pain or fatigue. As part of the overall cancer treatment plan, the patient’s medical oncologist oversees conventional treatment and integrative services.
When a patient is interested in integrative services, Pritt or another member of the cancer care team sends the practitioner(s) their contact information. The practitioner contacts the patient to schedule the services. As independent contractors, the practitioners do their own scheduling, reminders, and so forth.
Olson considers scheduling patients herself a key part of acupuncture treatment. “Often, patients want to talk about what’s bothering them,” she says. “I have to see them as a whole person, even when I’m scheduling, to help them.”
Promoting Integrative Services
About 90% of patients who use integrative services are referred to these services by members of the cancer care team. But patients can also learn about available integrative services on their own and ask to participate.
The Integrative Services Program describes available integrative services on its website, posts flyers throughout the cancer center, and hosts special events that promote integrative services. For example, the cancer center’s National Cancer Survivor Day includes activities such as yoga classes or an acupuncture session so patients can try integrative services.
Tracking Integrative Services
The Integrative Services Program currently tracks the use of integrative services, including:
- The number of patients who use integrative services
- Which services patients use
- The number of appointments or classes for each service
They do not track or measure outcomes.
James M Stockman Cancer Institute Implements Whole Person Cancer Care
Promoting Healing and Well-Being While Treating Cancer
The James M Stockman Cancer Institute has achieved the following results to date.
Integrative services are a routine part of cancer care at the James M Stockman Cancer Institute, demonstrating that community health systems can provide whole person cancer care.
“This is a shining example of how any community health systems with a strong leader that uses the right framework and systems and has a strong care team can actually do this,” says Dr. Jonas. “It takes leadership, persistence and working within the system to make sure there’s buy-in.”
Creating an integrative cancer institute, the model typically used by academic medical centers, is often infeasible for community health systems due to the high cost of establishing and managing the center and paying for staff. Instead, Dr. Mansky made integrative services a routine part of cancer care. This was easier and less expensive to implement and enabled the James M Stockman Cancer Institute to provide integrative services to more patients.
Patient and caregiver voices are included in care plans and to some extent, in programming. Most patients come to the intake appointments with a family member or friend. The intake process for new patients and ongoing assessments include personalized recommendations for integrative services. Patients and caregivers learn about and discuss available integrative services with members of the care team. Together, they decide which, if any, integrative services are a fit for the patient at that time.
The stakeholder group that helped develop the integrative services program included cancer survivors and patient advocates. Currently, the James M Stockman Cancer Institute obtains informal patient feedback about programming from members of the care team.
“My space is the lobby of the integrative area of the cancer institute, where patients come and go,” says Pritt. “I talk with them about their ideas and feedback.”
Brienne Superczynski, LCSW-C, an oncology social worker for breast cancer patients, says that she hears “absolute praise” from patients who use integrative services. Patients like the availability of the services and having easy access to them, as well as how the therapies and the environments make them feel. They also like the providers who are delivering the integrative services.
The institute also surveys patients about their experiences with integrative services; however, the response rate has been very low. The team is working on improving the process to obtain more feedback. For example, during visits, providers remind patients to complete the surveys.
Integrative services are anchored to “what matters” to the patient. The assessment and intake process at the James M Stockman Cancer Institute focuses on what matters to each patient in addition to treating their cancer. Oncology nurse navigators and social workers are trained in assessing patients for anxiety, depression, and fatigue.
The institute has also started to incorporate the Personal Health Inventory for Oncology and the HOPE note for oncology into their processes. HOPE stands for Healing-Oriented Practices & Environments. Both tools were developed by the Healing Works Foundation in collaboration with cancer centers that participated in the Integrative Oncology Leadership Collaborative.
Free Tools for Implementing Whole Person Cancer Care
Personal Health Inventory for Oncology (PDF)
Use this tool to better understand each patient, including the internal and external influences on their health and what they need to heal. It helps the team (and the patient) learn what is most important and identify areas to work on to improve health.
Integrative Oncology Solution Guide (PDF)
Use this resource-mapping tool to further identify areas your patients are ready to work on to improve their health and give them evidence-based information on how to do so. The solution guide covers:
- Nutrition
- Sleep
- Stress management
- Activity
- Social support
Review the results of the patient’s Personal Health Inventory for Oncology using the HOPE note for Oncology. Identify up to three items the patient wants to focus on. Provide resources and steps for taking action. Have a care team member reach out within two weeks to check in and provide support.
Recommended actions typically fall under:
- Educational handouts for self-care
- Referral to a technology tool or app
- Referral to an internal resource or specialist
- Referral to an outside community resource
The solutions guide includes instructions for customizing this tool for your cancer center.
The Healing Works Foundation’s whole person cancer care web page also includes links to journal articles, case studies, other tools, and more.
About 15% of cancer patients at the James M Stockman Cancer Institute use integrative services, compared to about 5% in academic medical centers. Convenience and staff support contribute to the high use of integrative services.
“Our integrative services are embedded within the structure of our oncology program,” says Dr. Mansky. “They are in the same building, steps away from where the patients are seen for oncology visits.”
“Our integrative services relieve pain and anxiety to help our patients get through every day better. Patients have to be able to get through the everyday to get through cancer treatment.”
— Brienne Superczynski, LCSW-C
While some patients may not initially understand or be interested in integrative services, continually hearing from physicians, nurse navigators, and social workers about the benefits of these services encourages patients to try them.
Anecdotal evidence shows that patients who use integrative services find relief from their symptoms and treatment side effects, relieve stress, improve their energy and mood, and use fewer drugs. Acupuncture, for example, helps minimize nausea, fatigue and neuropathy, according to Olson. It is also useful in relieving anxiety. Patients also report benefiting from the support provided by their integrative practitioners and other patients.
Challenges and Lessons Learned
Dr. Mansky and his team faced the following challenges in implementing whole person cancer care.
Lack of resources. As part of a community health system, the James M Stockman Cancer Institute did not have the resources and services of many academic centers providing whole person cancer care. Dr. Mansky could not follow the typical path of establishing an institute for whole person cancer care. Instead, he integrated whole person cancer care into routine cancer care.
Getting buy-in for integrative services from physicians. Before Dr. Mansky joined Frederick Health, cancer care had not emphasized integrative services. Through presentations and other educational events that focused on the scientific evidence supporting the use of integrative services in cancer and providing opportunities to try yoga and acupuncture, Dr. Mansky was able to get buy-in from physicians and leadership. He brought in consultants from the Healing Works Foundation to facilitate the education.
“Once our physicians understood that integrative services had a scientific underpinning and that our patients enjoyed these services, they were open to exploring this,” says Dr. Mansky.
Lack of space and staff to grow. There is no room within the cancer institute to provide more integrative services, which would also require more staff and administration support. This challenge remains to be solved.
Tips for Providing Whole Person Cancer Care in Community Health Systems
Develop a whole person cancer care approach that works for cancer programs in community health systems.
“Be aware of and understand the chemistry of community cancer programs,” says Dr. Mansky.
Talk to all stakeholders to assess knowledge of and interest in integrative services and involve community members in program planning. In the beginning, Dr. Mansky met with patients and their family members, physicians, and integrative practitioners in the community to learn their views about integrative services. In developing the approach, he worked with cancer survivors, patient advocates, and other community members.
“Community members want to see the community as becoming better. As long as they can be part of the process, you’ll find support,” says Dr. Mansky.
Focus on getting support from leaders. Lack of leadership support is a key challenge in implementing whole person cancer care. Although leaders at Frederick Health brought Dr. Mansky in to improve cancer services, he had to understand how those leaders viewed whole person cancer care and then demonstrate and advocate for his vision.
“You have to have some personnel who are at least open to making this happen,” he says. “If you have to drive against inertia and potentially resistance from the organization, it’s much more difficult.”
Embed whole person cancer care within the community cancer process. Academic centers that offer whole person cancer care usually have separate centers for integrative services. Community cancer institutes do not have the resources to do this, and patients who seek care at community cancer institutes want the convenience of all services being in one place.
Create a culture that supports integrative services. When leaders support integrative services and physicians, nurses, social workers, and other members of the cancer care team believe integrative services can help their patients, it is easier to implement these services. Also, patients are more likely to try integrative services when trusted members of their care team recommend them.
Choose the right integrative providers. The integrative services providers at the James M Stockman Cancer Institute live and work in the community. They helped structure the integrative services program and its administration and are very engaged.
“Our integrative providers are the backbone of our program,” says Pritt.
Take advantage of available free resources.
Free resources a key part of the business case for using a whole program cancer care approach. Take advantage of these resources to demonstrate the value of integrative services in cancer to leaders and to build a program based on evidence about what works best. Many free resources are available on the Healing Works Foundation website.
Visit A Whole Person Approach to Cancer Care at Healing Works Foundation to access free resources.
Next Steps
Expanding Integrative Services
Dr. Mansky and his team plan to enhance the processes and systems used in the integrative services program at the James M Stockman Cancer Institute, including collecting data to track outcomes that will help them highlight the effectiveness of the program.
Although space and administrative support for integrative services is limited, Dr. Mansky would like to expand integrative services to cancer survivors, family members, staff, and perhaps hospitalized patients.
Resources
Free Resources on Whole Person Cancer Care
A Whole Person Approach to Cancer Care, Healing Works Foundation:
- Personal Health Inventory for Oncology (PDF)
- Integrative Oncology Solution Guide (PDF)
- Other tools and resources
- Content on diagnosis, treatment, and survivorship
- Core reading
- Making Whole Person Cancer Care Routine and other case studies
Frederick Health
- James M Stockman Cancer Institute’s Integrative Services web page
References
- National Cancer Institute. Bringing Research to the Community to Reduce Cancer Disparities. (2017, September 21). www.cancer.gov/research/areas/disparities/chanita-hughes-halbert-clinical-trialscommunity-access.
- Sakallaris B. R., MacAllister L., Voss M., Smith K., & Jonas W.B. (2015). Optimal healing environments. Global Advances in Health and Medicine, 4(3), 40-5. doi.org/10.7453/gahmj.2015.043
Featured image by Bartłomiej Balicki on Unsplash
Topics: Integrative Health


