
Developing an Integrative Health Model: Who, What, and How
LETTER FROM DR. WAYNE JONAS
Dear Colleagues,
As primary physicians, our job is to keep our patients healthy, help them heal when sick or hurt, and reduce their suffering from chronic disease. Our challenge is that only 15 to 20 percent of a population’s health comes from medical care.
The other 80 percent is due to factors largely outside the health care system: social and environmental determinants of health, lifestyle and behavior, and evidence-based complementary approaches to healing.
Optimal health and healing involves coordinating these practices into the delivery of patient-centered, integrated, and team-delivered care. I call this integrative health – a system that makes use of all evidence-based tools for health, healing, and well-being. But how can we provide this?
By exploring and using an expanded set of tools – ones that involve listening to our patients and treating them in a holistic manner – we can fully understand their needs and values, match their goals with good practices, and help them heal and improve health and well-being.
This white paper provides a guide to integrating some of these tools into your practice. It highlights opportunities to develop relationships with alternative and allied health care providers to add evidence-based self-care and complementary medicine to your practice.
I begin with some basic practices that have reasonable evidence on safety and effectiveness. This is a dynamic paper, however, and as new science and guidelines emerge, I will add to the list of practices.
I hope you find it a useful road map for developing expertise in integrative health.

Yours in health,
Wayne Jonas, M.D.
UNDERSTANDING INTEGRATIVE HEALTH
This document is a guide to help physicians and other health care providers incorporate self-care and complementary approaches into their mainstream practice as they move toward person-centered, integrative health for improving patient outcomes and satisfaction while delivering a better quality of care.
 What is Integrative Health?
What is Integrative Health?
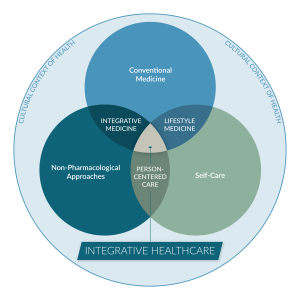
Integrative health is the pursuit of personal health and well-being foremost, while addressing disease as needed, with the support of a health team dedicated to all proven approaches – conventional, complementary and self-care.
Optimal health and well-being arises when we attend to all factors that influence healing including medical treatment, personal behaviors, mental and spiritual factors, and the social, economic, and environmental determinants of health.
Conventional medicine is the delivery of evidence-based approaches for disease prevention and treatment currently taught, delivered, and paid for by the mainstream health care system.
Integrative medicine is the coordinated delivery of conventional medicine combined with evidence-based complementary and alternative medicine (CAM) designed to enhance health and well-being.
Lifestyle medicine involves the incorporation of healthy, evidence-based self-care and behavioral approaches into conventional medical practice to enhance health and healing.
Thus, integrative health redefines the relationship between the practitioner and patient by focusing on the whole person and the whole community. It is informed by scientific evidence and makes use of all appropriate preventative, therapeutic, and palliative approaches, health care professionals, and disciplines to promote optimal health and well-being. This includes the coordination of conventional medicine, complementary/alternative medicine, and lifestyle/self-care.
SELF-CARE THOUGH BEHAVIORAL & LIFESTYLE CHANGE
Akey dimension of a person-centered, integrative health practice is assisting patients in making lifestyle, behavioral, and self-care changes. Multiple studies show that behaviors such as smoking cessation, moderate alcohol use, healthy food, regular exercise, and the social and emotional management of stress can prevent and even treat 70 percent of chronic disease. 1-2 Thus, these self-care approaches are the cornerstone of integrative health and good medicine.
Nutrition and yoga are two examples of self-care practices.
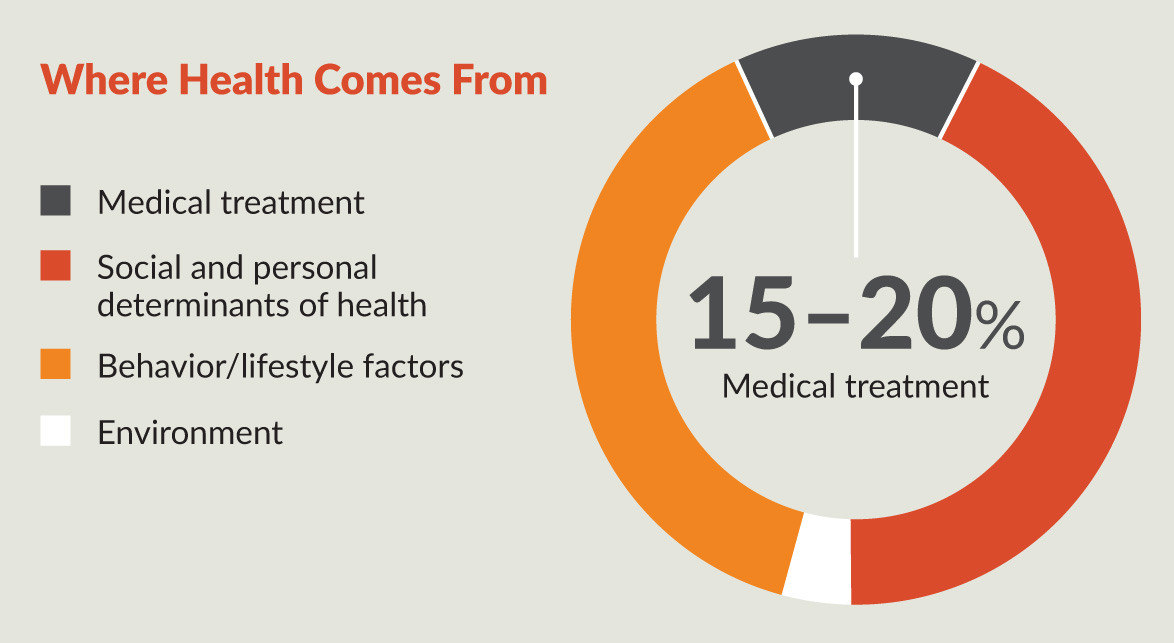
Modern medicine misses 80 percent of what’s needed to heal from chronic disease. 2a
NUTRITIONAL COUNSELING
What is it?
Nutrition is a key determinant in three of the top four causes of death – cardiovascular disease, stroke, and cancer – not to mention a key component of most chronic conditions primary care clinicians treat: diabetes, obesity, hypertension, and hyperlipidemia. 3 4
One survey of 451 family physicians found that 58.1 percent believed that more than 60 percent of their patients would benefit from nutritional counseling. Yet few provided the counseling or referred their patients to dietitians. 5
Few doctors receive training on nutrition or nutritional therapy in medical school or residency. In addition, nutritional counseling is time consuming, nearly impossible to fit into the typical 10- to 15-minute visit, and limited in insurance coverage. 3 6
A nutritional consult typically begins with a one-hour evaluation to assess the patient and the patient’s diet. The nutritionist may also assess the patient’s sleep patterns, physical activity, and other lifestyle factors, as these can affect eating.
With this information, the nutritionist works with the patient (or client) to identify opportunities for change. This doesn’t always mean starting a diet. It could mean identifying one adjustment – such as giving up soda or adding more fish, nuts, and vegetables – that can have an impact on health and healing.
Next is formulating a plan. For instance, if the patient doesn’t have time to cook and shop, options could include utilizing a service that delivers healthy food to the door or providing patients instruction on food selection when eating out. If a patient eats because of stress, then the nutritionist works with the patient to identify the underlying eating urges and identify strategies to manage them.
What does the science show?
Numerous studies find that improving diet can provide the same, if not better, benefits as medical therapy with less risk, fewer side effects, lower costs, and shorter hospital stays. 3 7 8 Most major medical guidelines incorporate recommendations for nutritional interventions and changes as an integral part of managing chronic disease.
The U.S. Preventive Services Task Force found good evidence that medium- to high-intensity dietary counseling for patients with hyperlipidemia and other risk factors for cardiovascular disease can produce medium to large changes in the intake of the core components of a healthy diet, particularly if delivered by nutritionists, dietitians, and specially trained primary health care professionals. 9 Similar studies have shown benefits for obesity, diabetes, and hypertension. 10-12
Not only can nutritional counseling improve a patient’s health, it can improve your reimbursement. Insurance is increasingly paying for nutritional counseling. In this age of value-based reimbursement, maintaining a patient’s health and preventing emergency department visits and hospitalizations – as well as readmissions – directly impacts compensation, whether you are salaried or have your own practice.
Whom should I refer?
Overweight or obese patients are obviously candidates for nutritional counseling, as are patients with diabetes, hypertension, and heart disease, as well as others at high risk for cardiovascular disease. Pregnant women, patients with chronic kidney disease, and patients with cancer may also benefit from referral.
Also consider referring patients with conditions such as HIV, cancer, and chronic obstructive pulmonary disease, who are at risk for significant weight loss.
How do I find a quality practitioner?
Check to see if the nutritionist is licensed or certified to practice. The primary organization of qualified nutrition professionals is the Academy of Nutrition and Dietetics. They provide a search by zip code on their website of qualified practitioners:
Look for a registered dietitian or registered dietitian nutritionist (RDN), disciplines that typically require a four-year bachelor’s degree and 900 to 1,200 hours in a dietetic internship through an accredited program, as well as passing a dietetics registration exam and continuing professional education requirements. Some RDNs are certified in a specialized area, including pediatrics nutrition, sports dietetics, nutrition support, and diabetes education.
Make sure the nutritionist you choose provides regular feedback on your patient, including nutritional recommendations and progress reports. In one survey of 235 family physicians, 54 percent said a lack of feedback compromises patient care. 13
Does insurance cover it?
Most commercial and government insurances, including Medicare and Medicaid, cover medical nutrition therapy (MNT) for certain conditions. Under Medicare, for instance, patients who have had a kidney transplant, or who have diabetes or kidney disease, can receive an initial nutrition and lifestyle assessment, one-on-one nutritional counseling, and follow-up visits to evaluate the patient’s progress. Obesity screening and counseling is covered if it is received in a primary care setting. Medicare recipients in rural areas may receive MNT through telehealth.
Precautions
Fad diets without evidence of benefit abound. Don’t let your patients be fooled by them. A large meta-analysis of major weight loss diets showed that over time (six to 12 months) all were equally effective if people adhered to them.14 The best diets to follow for general health are variations of the Mediterranean and DASH diets, which are based on the Alternate Healthy Eating Index. 15
Extreme dietary changes can harm your patients – both physically and psychologically. Cyclical weight loss and regain is bad for health and makes permanent weight loss more difficult. Implementing a major dietary change without medical monitoring and supervision can also get patients into trouble – especially if they are effective – as adjustments in medications or other therapies may be needed. Weight loss drugs and surgery are not recommended alone and should always be accompanied by diet and lifestyle changes. Thus, integrative health principles apply, such as person-centered care, shared decision making, and combining conventional medicine and self-care.
THERAPEUTIC YOGA
What is it?
You may not think of yoga as a medical intervention, but numerous studies attest to the benefits of the centuries-old mind/body practice on a wide range of health-related conditions, particularly stress, mental health, and pain management. 16
This has led to the development of a new form of yoga: therapeutic yoga, in which practitioners receive additional training in anatomy, physiology, psychology, and other medically related topics to provide personalized therapy to help their clients – your patients – manage chronic conditions.
Therapeutic yoga is officially described as the “application of yoga postures and practice to the treatment of health conditions to prevent, reduce, or alleviate structural, physiological, emotional, and spiritual pain, suffering, or limitations.” 16
Most therapeutic yoga professionals work or affiliate in hospital or clinical settings. 17
What does the science show?
Studies find therapeutic yoga practice can relieve stress, lower breathing rate, heart rate, blood pressure, and cortisol levels, as well as improve quality of life. 16 18-20 The stretching and flexibility that comes with yoga practice provides pain relief, with studies demonstrating its benefits in patients with arthritis, carpal tunnel syndrome, and back pain. It has also been shown to improve anxiety, obsessive-compulsive disorder, major depression, and insomnia. 21-27
A literature review of 120 studies on yoga found significant benefits reported in arthritis and other musculoskeletal disorders, as well as in cardiovascular endurance in healthy individuals. In patients with COPD and asthma, yoga programs focused on breath control and meditation significantly improve objective measures of lung function (FEV1, PERF, MVV, and FVC). 28
There is also good evidence that yoga practice mitigates risk factors for cardiovascular disease, including weight, blood pressure, and lipids. 28 Emerging evidence points to possible benefit in prevention of Alzheimer’s and other dementias, although more research is needed. 29 30
The medical evidence is strong enough that some of the best medical centers in the country now offer yoga therapy, including the University of Texas MD Anderson Cancer Center, Memorial Sloan Kettering Cancer Center, the Mayo Clinic and Cleveland Clinic. 17
Whom should I refer?
Therapeutic yoga has been studied in patients with the conditions listed previously, but also with cancer, irritable bowel syndrome, stroke, Type 2 diabetes, and neuromuscular conditions. 31-38 It is almost always used as an adjunctive intervention properly integrated into conventional medical care.
The most common conditions yoga therapists see are anxiety, back and neck pain, joint pain and stiffness, and hypertension. 39 40
How do I find a quality practitioner?
The International Association of Yoga Therapists (IAYT) sets educational standards (PDF) for the training of yoga therapists and accredits training facilities. Standards include 90 hours of training in anatomy and physiology, as well as 45 hours devoted to learning about commonly used drugs and surgical procedures they may encounter, common medical terminology, psychology, and mental health.
Overall, therapeutic yoga instructors must complete a minimum of 800 hours of training over two years, most which must be provided in person, not remotely. This includes a minimum of 205 hours as a practicum.
You can find members of IAYT here. The organization recently began a certification program.
Does insurance cover it?
It depends. Medicare, for instance, covers the Dean Ornish Program for Reversing Heart Disease, which incorporates yoga into a comprehensive lifestyle management approach when provided by a hospital as an intensive cardiac rehab program. 41 But few commercial insurance providers cover therapeutic yoga for, or under, other conditions. That may change as this young field matures.
Precautions
Overall, those who practice yoga have a low rate of side effects, and the risk of serious injury from yoga is quite low. However, certain types of stroke as well as pain from nerve damage are among the rare possible side effects of practicing yoga. Patients with chronic pain can be injured from too rapid or strenuous practice without supervision of a practitioner properly trained for these conditions.
Women who are pregnant and people with certain medical conditions, such as high blood pressure, glaucoma (a condition in which fluid pressure within the eye slowly increases and may damage the eye’s optic nerve), and sciatica (pain, weakness, numbing, or tingling that may extend from the lower back to the calf, foot, or even the toes) should modify or avoid some yoga poses.
COMPLEMENTARY & INTEGRATIVE MEDICINE
An estimated one in three U.S. adults uses some form of CAM, primarily in conjunction with conventional medicine rather than as a substitute. 42 When used to augment conventional medicine, it is referred to as complementary and integrative medicine or (CIM). CAM/CIM practices range from nutritional and herbal supplements to chiropractic care, massage, and acupuncture, as well as more ancient traditional practices such as Ayurveda and Traditional Chinese Medicine.
People with multiple chronic conditions may access an average of two CAM therapies a year. 43 For instance, one study of nearly 2,500 adults with diabetes found that 48 percent used CAM. 44 An even higher percentage of patients with cancer use CAM. 45
The U.S. Food and Drug Administration (FDA) and national medical societies such as the American College of Physicians have integrated CAM (along with self-care approaches) into their recommendations for treating chronic pain and stress-related conditions.
When properly integrated with conventional medical treatment, CAM practices form an important component of integrative medicine as described in this paper.
Major Health Systems Embrace Integrative Medicine Services
Large medical centers, including Stanford, Harvard, Yale, MD Anderson Cancer Center, Duke, the University of Arizona, Georgetown, and George Washington schools of medicine, have embraced integrative medicine as an evidence-based approach. A government-funded 2010 survey of more than 700 U.S. hospitals found that 49 percent of respondents primarily offered CAM because of patient demand, while another 24 percent said such services reflected their organizational mission. Other motivations included clinical effectiveness (45 percent), attracting new patients (41 percent), and differentiation from competitors (36 percent).
More than 70 U.S. academic health centers with integrative medicine programs are members of the Academic Consortium for Integrative Medicine & Health. There is a corresponding European Society of Integrative Medicine and a global International Society for Complementary Medicine Research. There is even an integrative medicine specialty designation through the American Board of Physician Specialties.
In addition, the National Institutes of Health (NIH) has funded the National Center for Complementary and Integrative Health, which is specifically focused on complementary and integrative health practices.
Yet research finds that patients and their families often do not discuss their use of CAM with their physicians, in part because they fear judgment and disapproval, and in part because their doctor never asks about it. Indeed, several studies find that physicians are often skeptical of CAM therapies and reluctant to recommend or even inquire about them with their patients. 46-49
If your patients aren’t telling you about their use of CAM and you don’t ask, then you are missing an important opportunity to protect them from harm, enhance their therapeutic options, and improve the quality of care you provide, and the ability to increase trust between you and your patient.
As the authors of a study on patient/physician communication about CAM noted:
“The fact that nearly half (44.5 percent) of patient encounters do not include CAM dialogue represents an unfortunately missed opportunity for patients and providers to take advantage of the ‘teachable moment’ of the clinic visit.” 50
Discussing CAM also fits within the shared decision making and patient-centered models of today – key
components of integrative health.
While many doctors think patients turn to CAM out of frustration with traditional medicine, that isn’t the case. Instead, patients view the two as complementary. In one survey of 831 adults who saw a medical doctor and used CAM, 79 percent felt the combination was more effective than either alone. Yet between 63 and 72 percent did not tell their doctor about at least one type of CAM they used. 51
Physicians increasingly understand the need to incorporate evidence-based CAM into their practice. One survey of 69 primary care physicians at a Texas academic medical center found that more than 68 percent believed that physicians should be knowledgeable about the most popular CAM approaches, 73.9 percent believed that patients’ spiritual beliefs and practices played an important role in healing, and 59.4 percent responded that several CAM therapies held promise for treating various symptoms and medical conditions. 52
The reality is that CAM is no longer considered “alternative,” but is an integral part of the whole person medical care patients require and increasingly want.
You may not be able to provide CAM in your own office, but you can refer. Here’s what you need to know about three of the most commonly used CAM approaches: acupuncture, chiropractic care, and massage. But first, some principles for why and how to refer to a CAM practitioner.
WHY AND HOW TO REFER FOR CAM/CIM
The Five Ps of Evidence-Based Integrative Medicine Practice
I have written about the basic principles to consider when considering referral or integrated use of CAM and conventional medicine. I call them the “Five Ps” – protect, permit, promote, partner, and payment. Your approach to all CAM (and conventional medicine) should be customized depending on the extent of evidence for safety and effectiveness of the treatment.
- Protect your patients from harmful treatments, including toxic treatments, poor quality or high-dose supplements, or unproven practices that replace proven care.
- Permit practices that are safe and might be effective, even if that effectiveness is partly due to placebo effects, provided they do not harm a patient’s quality of life or pocketbook.
- Promote practices, both CAM and conventional, that are proven safe and effective through high quality, randomized, controlled trials.
- Partner with patients. Sharing medicine is a cornerstone of person-centered care and should also be a guide in integrative medicine. Meaningfulness in medicine (for the patent and practitioner) is essential for optimal healing.
- Payment is key in accessing CAM approaches. Identify opportunities to help your patient gain coverage before recommending therapies.
Guides for Referral to CAM Practices
The preeminent textbook on Integrative Medicine, The Healing Encounter in Integrative Medicine, suggests that practitioners consider the following questions before prescribing or recommending any therapy: 53
- Does the therapy result in symptom resolution or suppression?
- What is the evidence?
- What is the potential harm?
- What is the cost?
- Does the therapy match the patient’s culture and belief system?
Once you deem it is appropriate to refer your patient: 54
- Discuss the patient’s preferences and expectations.
- Review safety and efficacy issues.
- Identify a suitable licensed provider by evaluating their training and credentials, approach to the specific problem your patient has, and patient cost.
- Provide the patient with key questions to ask the provider during the initial consultation.
- Schedule a follow-up visit (or telephone call) to review the treatment plan.
- Follow up to review the response to treatment.
- Provide documentation such as a one-sheet on the practice. (Many are available on DrWayneJonas.com.)
ACUPUNCTURE
What is it?
Acupuncture is an ancient Chinese healing system used by hundreds of millions of people throughout the world. Practitioners insert hair-thin needles into specific locations along the body’s “energy” meridians or points. The patient then lies still, often for 20 to 40 minutes, as the body responds.
The effects of acupuncture may be related to the analgesic effects of endogenous opioid release as well as the release of serotonin and norepinephrine antagonists that block the non-naloxone response. Imaging with MRI also finds involvement of the limbic system, hypothalamus, and brainstem networks. 55
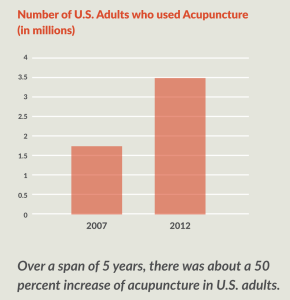 In 2012, about 3.5 million U.S. adults, or about 1.5 percent of the population, used acupuncture, a 50 percent increase in five years. 42 55 The most common reasons for its use are pain related – low back pain, joint pain, neck pain, and headache/migraine. About half of patients using acupuncture see it as a complementary approach to traditional medicine. 55
In 2012, about 3.5 million U.S. adults, or about 1.5 percent of the population, used acupuncture, a 50 percent increase in five years. 42 55 The most common reasons for its use are pain related – low back pain, joint pain, neck pain, and headache/migraine. About half of patients using acupuncture see it as a complementary approach to traditional medicine. 55
The practice is also increasingly being used by primary care physicians, anesthesiologists, and pain management
specialists, with several training programs specifically designed for physicians. 55
What does the science show?
There is good evidence on the effects of acupuncture for acute and certain types of chronic pain. The effect is more than placebo, although belief and positive expectations can improve the effects. An individual patient meta-analysis of 29 clinical trials involving nearly 18,000 patients with chronic pain (musculoskeletal, osteoarthritis of the knee, and headache/migraine) found modest but statistically significant differences between pain levels in those who received acupuncture versus those who received simulated (placebo) acupuncture. The authors concluded that the effects were clinically relevant, went beyond that of a placebo effect, and are “of major importance for clinical practice.” 56
A later analysis of the same data found that 90 percent of the benefits of acupuncture relative to controls was sustained at 12 months. 57 Both studies were funded by the NIH National Center for Complementary and Integrative Health and published in prominent mainstream, peer-reviewed journals.
A year-long, federally funded study also found that acupuncture may significantly reduce hot flashes and other menopause-related symptoms, including anxiety, memory/concentration, and sleep quality, with the benefits lasting at least six months after the acupuncture treatments ended. 58 Another study published in the Journal of the American Medical Association (JAMA) found that six weeks of electroacupuncture significantly improved stress urinary incontinence in the 252 women receiving the procedure compared to a similar group who received simulated (placebo) acupuncture without electrical current. 59
As Josephine P. Briggs, M.D., and David Shurtleff, Ph.D., of the National Center for Complementary and Integrative Health wrote in an editorial in JAMA after the study’s publication: “Clearly these ancient practices are helping reveal the complexity of the links between the mind and the body.” 60
Whom should I refer?
Research shows that acupuncture is effective for treating several conditions including:
- Low back pain.
- Stress urinary incontinence.
- Chemotherapy-induced nausea and vomiting.
- Headaches.
For the research on acupuncture’s effectiveness for specific medical conditions, visit the National Center for Complementary and Integrative Health.
How do I find a quality practitioner?
You can search for a physician who practices acupuncture in your area at the American Academy of Medical Acupuncture. Board certification requires graduation from an accredited medical school, license to practice medicine, and at least 300 hours of systemic acupuncture training, 100 hours of which are clinical training.
You can also search out non-M.D. practitioners. Most states and the District of Columbia require licensing for acupuncturists, with most designating licensed practitioners as “Licensed Acupuncturists,” “Acupuncture Physicians,” or “Doctors of Oriental Medicine.” You can find licensure requirements for your state here on the website of the National Certification Commission for Acupuncture and Oriental Medicine (NCCAOM), which is the main accreditation group for acupuncturists.
Does insurance cover it?
Most insurance does not cover acupuncture; however, some insurers offer discounts to certain providers and some plans have riders or supplements to their normal policies that cover acupuncture. Inquire if your plans can do this.
Precautions
Acupuncture is quite safe, and complications are rare when the method is properly delivered. The most important thing is ensuring the practitioner uses sterile, disposable needles and does not insert them in areas that can damage vital organs.
The FDA regulates acupuncture needles as medical devices for use by licensed practitioners and requires that needles be manufactured and labeled according to certain standards. For example, the FDA requires that needles be sterile, nontoxic, and labeled for single use by qualified practitioners only. 61
MASSAGE THERAPY
What is it?
A 2016 survey of 1,202 adults by the American Massage Therapy Association (AMTA), the largest nonprofit professional association for massage in the United States, found that nearly one in five people received a massage in the past year, half of them for medical reasons. The most common reasons were pain relief/pain management, soreness and stiffness, injury recovery, health and wellness, and pregnancy. Another third cited stress relief as the reason for their massage. The survey also found that 89 percent of consumers surveyed believed that massage can be effective in reducing pain, with 28 percent of respondents stating they have used massage therapy for pain relief. 62
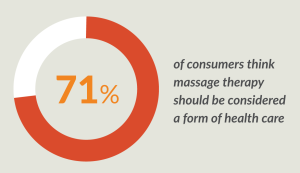 In 2016, 12 percent of patients were referred to a massage therapist by their doctor, and half (51 percent) said their doctor encouraged them to receive a massage. 62 Today, less than a third of consumers view massage as a form of pampering, and 71 percent think it should be considered a form of health care. 62
In 2016, 12 percent of patients were referred to a massage therapist by their doctor, and half (51 percent) said their doctor encouraged them to receive a massage. 62 Today, less than a third of consumers view massage as a form of pampering, and 71 percent think it should be considered a form of health care. 62
There are several types of massage, and a good therapist will work with your patient to identify the one that works best. These include: 63
- Swedish massage. This is the type most people think of when they think of massage. In Swedish massage, the therapist uses long strokes, kneading, deep circular movements, vibration, and tapping.
- Sports massage. This type combines techniques of Swedish massage and deep tissue massage to release chronic muscle tension.
- Myofascial trigger point therapy. This type focuses on trigger points – areas that are painful when pressed and are associated with pain elsewhere in the body.
What does the science show?
Studies find significant benefits of therapeutic massage for depression, osteoarthritis, chronic back and neck pain, chronic constipation, fibromyalgia, and headaches. 64-69 Preterm infants who receive massage demonstrate greater weight gain and immune function than those who do not. 70 A review of four clinical trials found that massage may improve quality of life for those with HIV, while several studies suggest massage may reduce pain, reduce stress, and improve mood in people with cancer. 71-73
Whom should I refer?
Patients with acute or chronic pain, those suffering from mental health disorders like depression and anxiety, and those who have conditions related to or exacerbated by stress can benefit.
How do I find a quality practitioner?
As of mid-2017, 44 states and the District of Columbia license massage therapists. 63 Many localities also require that massage therapists meet certain criteria, including licensing and certification.
You can learn what your state requires at the American Massage Therapy Association (AMTA) website, the largest nonprofit professional association for massage.
Look for a massage therapist who is board certified, which requires additional training and testing administered by the National Certification Board for Therapeutic Massage and Bodywork. The therapist is board certified if they have the initials “BCTMB” after their name.
Also, make sure they have trained with an accredited school. There are more than 300 in the United States. Several organizations accredit schools, including the he Commission on Massage Therapy Accreditation (COMTA), the National Accrediting Commission of Arts & Sciences (NACCAS), the Accrediting Commission of Career Schools and Colleges (ACCSC), and the Accrediting Bureau of Health Education Schools (ABHES).
The AMTA recommends at least 500 hours of supervised, in-class massage therapy training, which includes the study of anatomy and physiology. Some states, such as New York, require even more hours of training.
Does insurance cover it?
Massage may be covered if prescribed by a physician or chiropractic professional.
Precautions
Patients on blood thinners, those who bruise easily or have low platelet counts or bleeding disorders should avoid deep tissue massages. Pregnant women should make sure to see a therapist who provides prenatal massage, and patients with cancer should avoid deep pressure over the area of the malignancy. 63
CHIROPRACTIC
What is it?
Chiropractic care is one of the most popular and fastest growing forms of CAM in the United States. In 2012, nearly 20 million adults, (8.4 percent of the population), received some form of chiropractic or osteopathic manipulation. 42 A study published that year also found that about a third of patients with chronic back or neck pain turned to a chiropractor, with a survey from Consumer Reports a year later finding that 59 percent were highly satisfied compared to 55 percent who saw a physical therapist and 34 percent who saw a primary care physician. 74 75
 In recent years, chiropractic has expanded its scope of practice beyond just spine-focused. Many chiropractors today, particularly sports chiropractors, use treatment modalities beyond adjustments/manipulations, including electrical stimulation, ultrasound, cold laser, and soft tissue techniques (active release technique, Graston, myofascial release), and corrective exercises. Many of these practices have been integrated into mainstream systems – such as in military and veteran health care.
In recent years, chiropractic has expanded its scope of practice beyond just spine-focused. Many chiropractors today, particularly sports chiropractors, use treatment modalities beyond adjustments/manipulations, including electrical stimulation, ultrasound, cold laser, and soft tissue techniques (active release technique, Graston, myofascial release), and corrective exercises. Many of these practices have been integrated into mainstream systems – such as in military and veteran health care.
Some have expanded even beyond that to nutrition counseling and dietary supplements; however, these are controversial and usually not accepted or integrated into mainstream health care.
What does the science show?
The evidence around chiropractic care has gotten stronger in recent years. A 2017 systematic review published in JAMA looked at 15 randomized, controlled trials involving more than 1,700 patients. The authors found that spinal manipulation resulted in an objective, clinically significant improvement in pain by about 10 points on the 100-point scale – a treatment response similar to that seen with non-steroidal anti-inflammatories.76 Another review published that year in Annals of Internal Medicine found similar results. 77 Neither found any evidence of serious adverse events.
In February 2017, the American College of Physicians released new guidelines for the treatment of subacute back pain, recommending that patients try non-pharmacologic therapies, including massage, acupuncture, and/or spinal manipulation as a first-line therapy. 78
Whom should I refer?
The strongest evidence for the benefits of spinal manipulation are for back pain. However, a systematic review of studies also found benefit in patients with fibromyalgia. 79
Chiropractors who use techniques beyond spinal adjustments, such as sports chiropractors, can also see patients with other musculoskeletal injuries, including iliotibial syndrome, plantar fasciitis, shoulder impingement, adhesive capsulitis, and elbow tendinitis. These professionals often work closely with orthopedic surgeons and physical therapists.
How do I find a quality practitioner?
Look for a practitioner who is a doctor of chiropractic (DC). They have completed four years of a doctoral graduate school program in a nationally accredited program that requires at least 4,300 hours of classroom, laboratory, and clinical internship. Most will also have completed a pre-med program in undergraduate school. While the profession is strongly associated with the spine, students receive extensive training in physical diagnosis, learning how to conduct abdominal, lung, heart, and even reproductive exams as some systemic conditions can mimic musculoskeletal complaints.
All states license chiropractors. Most states designate chiropractors as physician-level providers and all require licensure. The National Board of Chiropractic Examiners (NBCE) oversees certification and licensure, and chiropractors must complete continuing education each year to maintain their licenses.
Although chiropractors are licensed, they are not allowed to write prescriptions for drugs, including anti-inflammatories, in most states.
Does insurance cover it?
Yes. Most insurance plans, including Medicare and some Medicaid plans, as well as most military and federal employee plans, cover chiropractic care. 80
Precautions
Be wary of chiropractors who put patients on long-term therapy, i.e., three times a week for 12 weeks. These are “high-volume” practices and the clinician tends to spend just a few minutes with the patient. Also, x-rays are rarely necessary, yet some chiropractors still order them. Some chiropractors have also ventured into “holistic” care that involves unproven electromagnetic devices and dietary supplements. Patients should be wary of these practices also.
Although there has been some concern about the risk of vertebrobasilar artery system (VBA) stroke after chiropractic care, a case control study of 1,829 VBA stroke cases occurring in a commercially insured and Medicare Advantage population found no significant association with manipulation. 81
REFERENCES
- McGinnis JM, Williams-Russo P, Knickman JR. The case for more active policy attention to health promotion. Health Aff (Millwood). 2002;21(2):78-93.
- McGinnis JM, Foege WH. Actual causes of death in the United States. JAMA. 1993;270(18):2207-2212.
2a. McGinnis JM, Williams-Russo P, Knickman JR. The Case For More Active Policy Attention To Health Promotion. Health Aff (Millwood). 2002 Mar-Apr;21(2):78-93. doi: 10.1377/hlthaff.21.2.78 - Kris-Etherton PM, Akabas SR, Bales CW, et al. The need to advance nutrition education in the training of health care professionals and recommended research to evaluate implementation and effectiveness. Am J Clin Nutr. 2014;99(5 Suppl):1153s-1166s.
- Crustolo AM, Ackerman S, Kates N, Schamehorn S. Integrating nutrition services into primary care: Experience in Hamilton, Ont. Can Fam Physician. 2005;51:1647-1653.
- Wynn K, Trudeau JD, Taunton K, Gowans M, Scott I. Nutrition in primary care: current practices, attitudes, and barriers. Can Fam Physician. 2010;56(3):e109-116.
- Nicholas LG, Pond CD, Roberts DC. Dietitian-general practitioner interface: a pilot study on what influences the provision of effective nutrition management. Am J Clin Nutr. 2003;77(4 Suppl):1039s-1042s.
- Rosen BS, Maddox PJ, Ray N. A position paper on how cost and quality reforms are changing healthcare in
America: focus on nutrition. JPEN J Parenter Enteral Nutr. 2013;37(6):796-801. - Kris-Etherton PM, Akabas SR, Douglas P, et al. Nutrition competencies in health professionals’ education and
training: a new paradigm. Adv Nutr. 2015;6(1):83-87. - Lin JS, O’Connor E, Evans CV, Senger CA, Rowland MG, Groom HC. Behavioral counseling to promote a healthy lifestyle in persons with cardiovascular risk factors: a systematic review for the U.S. Preventive Services Task Force. Ann Intern Med. 2014;161(8):568-578.
- Knowler WC, Barrett-Connor E, Fowler SE, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346(6):393-403.
- Diabetes Prevention Program Research G, Knowler WC, Fowler SE, et al. 10-year follow-up of diabetes incidence and weight loss in the Diabetes Prevention Program Outcomes Study. Lancet. 2009;374(9702):1677-1686.
- Caraci F, Leggio GM, Salomone S, Drago F. New drugs in psychiatry: focus on new pharmacological targets.
F1000Research. 2017;6:397. - Kuppersmith NC, Wheeler SF. Communication between family physicians and registered dietitians in the outpatient setting. J Am Diet Assoc. 2002;102(12):1756-1763.
- Anderson JW, Konz EC, Frederich RC, Wood CL. Long-term weight-loss maintenance: a meta-analysis of US studies. The American Journal of Clinical Nutrition. 2001;74(5):579-584.
- Sotos-Prieto M, Bhupathiraju SN, Mattei J, et al. Association of Changes in Diet Quality with Total and Cause-Specific Mortality. N Engl J Med. 2017;377(2):143-153.
- Woodyard C. Exploring the therapeutic effects of yoga and its ability to increase quality of life. Int J Yoga. 2011;4(2):49-54.
- Enfield S. Why More Western Doctors Are Now Prescribing Yoga Therapy. February 3, 2016. https://www.yogajournal.com/lifestyle/western-doctors-prescribing-yoga-therapy.
- Granath J, Ingvarsson S, von Thiele U, Lundberg U. Stress management: a randomized study of cognitive behavioural therapy and yoga. Cogn Behav Ther. 2006;35(1):3-10.
- Bharshankar JR, Bharshankar RN, Deshpande VN, Kaore SB, Gosavi GB. Effect of yoga on cardiovascular system in subjects above 40 years. Indian J Physiol Pharmacol. 2003;47(2):202-206.
- Oken BS, Zajdel D, Kishiyama S, et al. Randomized, controlled, six-month trial of yoga in healthy seniors: effects on cognition and quality of life. Altern Ther Health Med. 2006;12(1):40-47.
- Woolery A, Myers H, Sternlieb B, Zeltzer L. A yoga intervention for young adults with elevated symptoms of
depression. Altern Ther Health Med. 2004;10(2):60-63. - Cohen L, Warneke C, Fouladi RT, Rodriguez MA, Chaoul-Reich A. Psychological adjustment and sleep
quality in a randomized trial of the effects of a Tibetan yoga intervention in patients with lymphoma. Cancer.
2004;100(10):2253-2260. - Kolasinski SL, Garfinkel M, Tsai AG, Matz W, Van Dyke A, Schumacher HR. Iyengar yoga for treating symptoms of osteoarthritis of the knees: a pilot study. J Altern Complement Med. 2005;11(4):689-693.
- Javnbakht M, Hejazi Kenari R, Ghasemi M. Effects of yoga on depression and anxiety of women. Complement Ther Clin Pract. 2009;15(2):102-104.
- Garfinkel MS, Singhal A, Katz WA, Allan DA, Reshetar R, Schumacher HR, Jr. Yoga-based intervention for
carpal tunnel syndrome: a randomized trial. JAMA. 1998;280(18):1601-1603. - Shannahoff-Khalsa DS, Ray LE, Levine S, Gallen CC, Schwartz BJ, Sidorowich JJ. Randomized controlled trial of yogic meditation techniques for patients with obsessive compulsive disorder. CNS Spectr. 1999;4(12):34-47.
- Shannahoff-Khalsa DS, Beckett LR. Clinical case report: efficacy of yogic techniques in the treatment of obsessive compulsive disorders. Int J Neurosci. 1996;85(1-2):1-17.
- Raub JA. Psychophysiologic effects of Hatha Yoga on musculoskeletal and cardiopulmonary function: a literature review. J Altern Complement Med. 2002;8(6):797-812.
- Khalsa DS, Stauth C. Brain longevity: The breakthrough medical program that improves your mind and memory. New York, NY: Grand Central Publishing; 2001.
- Khalsa DS. Integrated medicine and the prevention and reversal of memory loss. Altern Ther Health Med.
1998;4(6):38-43. - Cote A, Daneault S. Effect of yoga on patients with cancer: our current understanding. Can Fam Physician.
2012;58(9):e475-479. - Huang AJ, Rowen TS, Abercrombie P, et al. Development and Feasibility of a Group-Based Therapeutic Yoga Program for Women with Chronic Pelvic Pain. Pain Med. 2017.
- McCall M, Thorne S, Ward A, Heneghan C. Yoga in adult cancer: an exploratory, qualitative analysis of the patient experience. BMC Complement Altern Med. 2015;15:245.
- Muhammad CM, Moonaz SH. Yoga as Therapy for Neurodegenerative Disorders: A Case Report of
Therapeutic Yoga for Adrenomyeloneuropathy. Integr Med (Encinitas). 2014;13(3):33-39. - Rogers KA, MacDonald M. Therapeutic Yoga: Symptom Management for Multiple Sclerosis. J Altern Complement Med. 2015;21(11):655-659.
- Ross Zahavich AN, Robinson JA, Paskevich D, Culos-Reed SN. Examining a therapeutic yoga program for prostate cancer survivors. Integr Cancer Ther. 2013;12(2):113-125.
- Schmid AA, Miller KK, Van Puymbroeck M, DeBaun Sprague E. Yoga leads to multiple physical improvements after stroke, a pilot study. Complement Ther Med. 2014;22(6):994-1000.
- Vizcaino M. Hatha yoga practice for type 2 diabetes mellitus patients: a pilot study. Int J Yoga Therap.
2013(23):59-65. - Sullivan M, Leach M, Snow J, Moonaz S. The North American yoga therapy workforce survey. Complement Ther Med. 2017;31:39-48.
- Ross A, Touchton-Leonard K, Yang L, Wallen G. A National Survey of Yoga Instructors and their Delivery of Yoga Therapy. Int J Yoga Therap. 2016;26(1):83-91.
- Centers for Medicare and Medicaid Services. Decision Memo for Intensive Cardiac Rehabilitation (ICR) Program – Dr. Ornish’s Program for Reversing Heart Disease (CAG-00419N) 2010; https://www.cms.gov/medicare-coverage-database/details/nca-decision-memo.aspx?NCAId=240&ver=7&NcaName=Intensive+Cardiac+Rehabilitation+(ICR)+Program+-+Dr.+Ornish%27s+Program+for+Reversing+Heart+Disease&bc=ACAAAAAAIAAA&siteTool=Medic. Accessed June 8, 2017.
- Clarke T, Black LI, Stussman BJ, et al. Trends in the Use of Complementary Health Approaches Among Adults: United States, 2002–2012. Centers for Disease Control and Prevention,;2015.
- Falci L, Shi Z, Greenlee H. Multiple Chronic Conditions and Use of Complementary and Alternative Medicine
Among US Adults: Results From the 2012 National Health Interview Survey. Prev Chronic Dis. 2016;13:E61. - Garrow D, Egede LE. Association between complementary and alternative medicine use, preventive care practices, and use of conventional medical services among adults with diabetes. Diabetes Care. 2006;29(1):15-19.
- Mao JJ, Farrar JT, Xie SX, Bowman MA, Armstrong K. Use of complementary and alternative medicine and prayer among a national sample of cancer survivors compared to other populations without cancer. Complement Ther Med. 2007;15(1):21-29.
- Ernst E, Posadzki P. Alternative therapies for asthma: are patients at risk? Clin Med (Lond). 2012;12(5):427-429.
- Stub T, Quandt SA, Arcury TA, Sandberg JC, Kristoffersen AE. Complementary and conventional providers in cancer care: experience of communication with patients and steps to improve communication with other providers. BMC Complement Altern Med. 2017;17(1):301.
- Stub T, Quandt SA, Arcury TA, et al. Perception of risk and communication among conventional and complementary health care providers involving cancer patients’ use of complementary therapies: a literature review. BMC Complement Altern Med. 2016;16:353.
- Jou J, Johnson PJ. Nondisclosure of Complementary and Alternative Medicine Use to Primary Care Physicians: Findings From the 2012 National Health Interview Survey. JAMA internal medicine. 2016;176(4):545-546.
- Zhang Y, Peck K, Spalding M, Jones BG, Cook RL. Discrepancy between patients’ use of and health providers’
familiarity with CAM. Patient Educ Couns. 2012;89(3):399-404. - Eisenberg DM, Kessler RC, Van Rompay MI, et al. Perceptions about complementary therapies relative to conventional therapies among adults who use both: results from a national survey. Ann Intern Med. 2001;135(5):344-351.
- Zhang Y, Peck K, Spalding M, Xu T, Ragain M. A study to examine the attitudes, knowledge, and utilization of CAM by primary care professional in West Texas. Complement Ther Med. 2010;18(6):227-232.
- Rakel D. The Healing Encounter in Integrative Medicine 4th edition. Elsevier; 2017.
- Institute of Medicine. Complementary and Alternative Medicine in the United States. 2005.
- Mao JJ, Kapur R. Acupuncture in primary care. Prim Care. 2010;37(1):105-117.
- Vickers AJ, Cronin AM, Maschino AC, et al. Acupuncture for chronic pain: individual patient data meta-analysis. Arch Intern Med. 2012;172(19):1444-1453.
- MacPherson H, Vertosick EA, Foster NE, et al. The persistence of the effects of acupuncture after a course of
treatment: a meta-analysis of patients with chronic pain. Pain. 2017;158(5):784-793. - Avis NE, Coeytaux RR, Isom S, Prevette K, Morgan T. Acupuncture in Menopause (AIM) study: a pragmatic,
randomized controlled trial. Menopause. 2016;23(6):626-637. - Liu Z, Liu Y, Xu H, et al. Effect of electroacupuncture on urinary leakage among women with stress urinary
incontinence: A randomized clinical trial. JAMA. 2017;317(24):2493-2501. - Briggs JP, Shurtleff D. Acupuncture and the complex connections between the mind and the body. JAMA.
2017;317(24):2489-2490. - National Center for Complementary and Integrative Health. Acupuncture: In Depth. 2017; https://nccih.nih.gov/health/acupuncture/introduction – hed4. Accessed July 11, 2017.
- American Massage Therapy Association. Consumer Views & Use of Massage Therapy. 2017; https://www.amtamassage.org/research/Consumer-Survey-Fact-Sheets.html. Accessed June 7, 2017.
- National Center for Complementary and Integrative Health. Massage Therapy for Health Purposes. 2017; https://nccih.nih.gov/health/massage/massageintroduction.htm – hed2. Accessed June 11, 2017.
- Cherkin DC, Sherman KJ, Kahn J, et al. A comparison of the effects of 2 types of massage and usual care on chronic low back pain: a randomized, controlled trial. Ann Intern Med. 2011;155(1):1-9.
- Kalichman L. Massage therapy for fibromyalgia symptoms. Rheumatol Int. 2010;30(9):1151-1157.
- Poland RE, Gertsik L, Favreau JT, et al. Open-label, randomized, parallel-group controlled clinical trial of
massage for treatment of depression in HIV-infected subjects. J Altern Complement Med. 2013;19(4):334-340. - Perlman AI, Ali A, Njike VY, et al. Massage therapy for osteoarthritis of the knee: a randomized dose-finding trial. PLoS One. 2012;7(2):e30248.
- Sinclair M. The use of abdominal massage to treat chronic constipation. J Bodyw Mov Ther. 2011;15(4):436-445.
- Plastaras CT, Schran S, Kim N, et al. Complementary and alternative treatment for neck pain: chiropractic,
acupuncture, TENS, massage, yoga, Tai Chi, and Feldenkrais. Phys Med Rehabil Clin N Am. 2011;22(3):521-537, ix. - Bennett C, Underdown A, Barlow J. Massage for promoting mental and physical health in typically developing infants under the age of six months. The Cochrane database of systematic reviews. 2013(4):CD005038.
- Hillier SL, Louw Q, Morris L, Uwimana J, Statham S. Massage therapy for people with HIV/AIDS. The Cochrane database of systematic reviews. 2010(1):CD007502.
- Corbin L. Safety and efficacy of massage therapy for patients with cancer. Cancer Control. 2005;12(3):158-164.
- Listing M, Krohn M, Liezmann C, et al. The efficacy of classical massage on stress perception and cortisol
following primary treatment of breast cancer. Archives of women’s mental health. 2010;13(2):165-173. - Martin BI, Gerkovich MM, Deyo RA, et al. The association of complementary and alternative medicine use and health care expenditures for back and neck problems. Med Care. 2012;50(12):1029-1036.
- Relief for your aching back: what worked for our readers. Consum Rep. March 17, 2017. http://www.consumerreports.org/cro/2013/01/relief-for-your-aching-back/index.htm. Accessed June 12, 2017.
- Paige NM, Miake-Lye IM, Booth MS, et al. Association of Spinal Manipulative Therapy With Clinical Benefit and Harm for Acute Low Back Pain: Systematic Review and Meta-analysis. JAMA. 2017;317(14):1451-1460.
- Chou R, Deyo R, Friedly J, et al. Nonpharmacologic Therapies for Low Back Pain: A Systematic Review for an
American College of Physicians Clinical Practice Guideline. Ann Intern Med. 2017;166(7):493-505. - Qaseem A, Wilt TJ, McLean RM, Forciea MA. Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain: A Clinical Practice Guideline From the American College of Physicians. Ann Intern Med. 2017;166(7):514-530.
- Schneider M, Vernon H, Ko G, Lawson G, Perera J. Chiropractic management of fibromyalgia syndrome: a
systematic review of the literature. J Manipulative Physiol Ther. 2009;32(1):25-40. - American Chiropractic Association. Insurance Coverage of Chiropractic: Quick Facts. https://www.acatoday.org/Patients/Access-Coverage/Insurance-Coverage. Accessed June 11, 2017.
- Kosloff TM, Elton D, Tao J, Bannister WM. Chiropractic care and the risk of vertebrobasilar stroke: results of a case control study in U.S. commercial and Medicare Advantage populations. Chiropr Man Therap. 2015;23:19.
CONTRIBUTORS
Contributors advised the creation of this paper, but the product is the work of the author and not necessarily a reflection of the contributors nor their organizations.
Jessica Donze Black, RD, MPH
Vice President of Community Health
The American Heart Association
Audrey N. Schoomaker, BSN, E-RYT
Owner, Myndwell LLC
ABOUT THE AUTHOR – DR. WAYNE JONAS
Dr. Jonas is a practicing family physician, an expert in integrative health and whole person care delivery, and a widely published scientific investigator. Dr. Jonas is the president of Healing Works Foundation. Additionally, Dr. Jonas is a retired lieutenant colonel in the Medical Corps of the United States Army.
Dr. Jonas was the director of the Office of Alternative Medicine at the National Institutes of Health (NIH) from 1995-1999, and prior to that served as the Director of the Medical Research Fellowship at the Walter Reed Army Institute of Research. He is a Fellow of the American Academy of Family Physicians.
His research has appeared in peer-reviewed journals such as the Journal of the American Medical Association, Nature Medicine, Journal of Family Practice, Annals of Internal Medicine, and The Lancet. Dr. Jonas received the 2015 Pioneer Award from the Integrative Healthcare Symposium, the 2007 America’s Top Family Doctors Award, the 2003 Pioneer Award from the American Holistic Medical Association, the 2002 Physician Recognition Award of the American Medical Association, and the 2002 Meritorious Activity Prize from the International Society of Life Information Science in Chiba, Japan.
Photo by Yoann Boyer on Unsplash
Topics: Behavior & Lifestyle | Complementary Medicine | Integrative Health
