What is Whole Person Primary Care
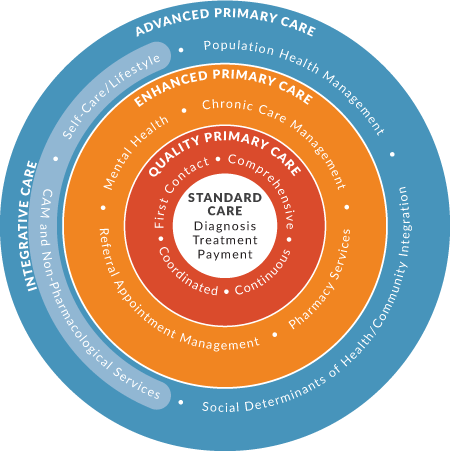
Whole person primary care is just good medicine. It is person-centered, relationship-based care, and it takes into account the social, spiritual, emotional, and behavioral aspects of health as well as the environment in which the person lives.
To be effective, whole person care must use an integrative approach that coordinates the delivery of evidence-based conventional medical care, complementary medicine, and lifestyle medicine within a primary care practice.
Incorporating a whole person approach into mainstream primary care practices enables physicians, nurses, and other health care providers to:
- Deliver higher quality advanced primary care.
- Improve patient outcomes and satisfaction.
- Lower costs.
- Reduce burnout.
Latest Blog Post
Rural health care presents unique challenges and opportunities that require thoughtful approaches. As clinicians, we can make significant impacts on rural health outcomes by considering patients' whole health—body, mind, and spirit. Understanding Rural Health Care…

Easy Access Personal Health Inventory for Your Practice
Your practice can use this online platform to help understand your patient and the internal and external influences on their health.
How does whole person care work in practice?
If you are interested in practicing whole person primary care, each one of these case studies shows one tool or method to try in your practice.
Now Available
“Healing and Cancer: A Guide to Whole Person Cancer Care” written by Alyssa McManamon, MD, and Wayne Jonas, MD published by Rodin Books, distributed by Simon and Schuster.
“Healing and Cancer” is intended to be read and actively used by teams caring for people with cancer and by caregivers and patients themselves to enhance healing, health, and wellbeing. “Healing and Cancer” directs readers to the best tools and resources available so that oncologists, primary clinicians, nurses, social workers, integrative practitioners, cancer care teams, patients with cancer and their caregivers, can incorporate whole person care into their own healing journey.