
Managing Hypertension Beyond Medication
LETTER FROM DR. WAYNE JONAS
High blood pressure (hypertension) is the largest preventable and treatable risk factor for chronic disease in the world. More than 119 million people in the United States – half of all adults – and more than 1 billion (1 in 3 adults) in the world have hypertension. 1, 2It is a major risk factor for stroke, heart attack, heart failure and kidney failure. However, because it rarely causes symptoms, many people don’t know they have it, while many who have it do not control it adequately.
Lifestyle is an important contributor to hypertension and equally important in managing it. In addition, medications are also effective for preventing and treating hypertension when they are properly integrated.
No one wants to hear the doctor say, “You have high blood pressure.” Receiving this diagnosis can seem overwhelming. When I tell a patient he or she has hypertension, it’s often received with a bit of fear, confusion and frustration. Some patients think I am telling them they are tense or stressed, but while stress can contribute to hypertension, the condition is actually an indication of the pressure of blood flow through their blood vessels as well as stiffness of those vessels. Hypertension affects many areas of a person’s life, including what to eat, how to move, how to sleep and how to manage stress.
The number of people receiving the diagnosis is increasing. In 2017, the American Heart Association changed the definition of normal blood pressure from 140/90 to 130/80.3 The European Society of Hypertension concurs with this definition for adults at high risk for cardiac problems. For other adults, ESH uses age-based guidelines with 140/90 as the norm. 4
To help you sort through the confusion and work with your doctor to develop a whole person approach, we provided this guide to hypertension. Regardless of the number used, it can help keep your blood pressure under control and your health intact.
Our focus is on whole person health – a combination of medication, complementary approaches and selfcare to manage hypertension and potentially reverse this chronic condition. Just make sure you involve your health care provider in any changes you make.

Be well,
Wayne Jonas, MD
HYPERTENSION
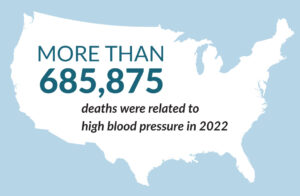
They call hypertension “the silent killer” for a reason. There are no symptoms, yet this condition – commonly known as high blood pressure – is a major contributor to deaths from cardiovascular and kidney diseases and stroke.5 Indeed, more than 685,875 deaths were related to high blood pressure in 2022. 6, 7
Hypertension is epidemic. Nearly half of all American adults have hypertension according to the 130/80 blood pressure standards set in 2017, or almost 120 million people. 8
And it’s only going to get worse. According to the American Heart Association, high blood pressure is expected to rise from 51% in 2020 to 61% by 2050. 9 This means that a larger portion of the U.S. population will be dealing with hypertension, which could lead to an increase in related health issues such as heart disease and stroke.
 According to a well-known study called the Framingham Heart Study, the risk of developing hypertension is about 90% for both men and women aged 55 to 65. This means that 9 out of 10 middle-aged adults with a normal lifestyle will eventually develop high blood pressure. 10
According to a well-known study called the Framingham Heart Study, the risk of developing hypertension is about 90% for both men and women aged 55 to 65. This means that 9 out of 10 middle-aged adults with a normal lifestyle will eventually develop high blood pressure. 10
However, if you treat hypertension with medication, lifestyle changes and complementary approaches, you can significantly reduce the risk of stroke, cardiovascular disease and other hypertension-related complications, including death. While high blood pressure can run in families, it’s also true that for many of us, lifestyle approaches alone can help prevent developing this condition in the first place. 11
Our hope is that this guide will help you understand your own risk of hypertension and, if you do have this condition, find ways to bring it under control.
BLOOD PRESSURE DEFINED
Blood pressure is the force of blood pushing against your arteries. These are the blood vessels that carry blood from your heart to all the other parts of your body. Your blood pressure measurement actually includes two numbers:
- Systolic blood pressure – The first number you will see. For example, a normal systolic blood pressure by US guidelines is 130 or lower. Your systolic blood pressure measures how much force your heart creates when it squeezes, or contracts, to push blood out.
- Diastolic blood pressure – The second number you will see. For example, a normal diastolic blood pressure by US guidelines is 80 or lower. Your diastolic blood pressure measures how much pressure is exerted on the walls of your arteries when your heart relaxes to allow blood back in.
As an example, Maria’s blood pressure is 120/70. When her heart squeezes to push blood to the rest of her body, the force is 120. This is a healthy level, below normal. When her heart relaxes to allow blood back in, the force is 70. This is also healthy and below normal.
Garrett’s blood pressure is 155/93. When his heart squeezes, it creates a lot of pressure on his artery walls, 25 points above the normal pressure of 130. When his heart relaxes, there is still quite a bit of pressure on his artery walls, 3 points above the normal US level.
When your blood pressure is high, it forces the heart to work harder, eventually weakening it and leading to heart failure. High blood pressure also causes other changes:
- It thickens blood vessel walls, which limits how much blood can flow through them at a time.
- It raises your risk of developing blood clots, which can cut off the flow of blood temporarily.
- It weakens blood vessels, increasing the risk that they will burst and bleed into your body.
- It lowers the amount of blood flowing to your brain. This raises your risk for stroke and dementia.
The damage to blood vessels from high blood pressure also contributes to kidney disease and kidney failure, raising your risk of needing dialysis (artificial filtering of the blood, which is done when your kidneys are not working) or a kidney transplant.
High blood pressure can also damage the tiny blood vessels in your eyes, raising the risk of blindness. It can harm your sex life by damaging blood vessels, and cause you to lose bone by making your body get rid of more calcium, which you need to maintain strong bone.
RISK FACTORS FOR HYPERTENSION
Hypertension affects men and women equally). Things that raise your risk include: 11
- Drinking a lot of alcohol
- Lack of physical activity
- Older age (before 55, men are more likely than women to have high blood pressure. Women are more likely to develop high blood pressure after menopause). 12
- Family history – Some people have a genetic risk of high blood pressure
- Diet high in sodium (salt) and low in potassium, a mineral found in bananas, potatoes, beans, yogurt and other whole foods.
- Stress levels
- Race – American-born Black people tend to have more hypertension than people in other ethnic groups.
Being overweight is one of the greatest risk factors for hypertension. It also makes the condition far more difficult to treat, particularly since carrying excess weight can cause other conditions such as diabetes, sleep apnea and inflammation. 7
Hypertension that Runs in the Family
So you’re not overweight, you exercise regularly and you follow a healthy diet. But you still have high blood pressure. Why?
The reality is that certain people simply have a genetic tendency for hypertension. That doesn’t mean you’re doomed to have it. If you know that hypertension runs in your family, you must be extra vigilant about following a healthy lifestyle and getting regular blood pressure checks. I recommend you buy a home blood pressure monitor and use it regularly. The American Heart Association has information on home blood pressure monitoring. 14
The American Heart Association and the American College of Cardiology, together with nine other major medical organizations, released guidelines in late 2017 for the prevention, detection and treatment of hypertension. While similar to older versions, the 2017 guidelines base treatment not just on your blood pressure numbers, but also on your overall risk of narrowed or blocked arteries, a condition called atherosclerotic cardiovascular disease (ASCVD). 15
Additionally, the 2023 European Society of Hypertension guidelines emphasize the importance of out-of-office blood pressure monitoring, such as home monitoring, along with traditional in-office measurements. This helps provide a more accurate picture of your blood pressure over time. 4
Both sets of guidelines continue to stress the importance of lifestyle changes (like diet, exercise, and weight management) and medication when necessary to manage blood pressure effectively.
The 2017 guidelines set a blood pressure goal of less than 130/80 for everyone, regardless of any other medical conditions or age. While not all medical professionals agree with this lower number, everyone agrees that no adult should have a blood pressure higher than 140/90. 4
Table 1 highlights the current US definitions of hypertension and recommended management.
TABLE 1: Blood Pressure Management Recommendations Based on 2017 US Guidelines
| BLOOD PRESSURE CATEGORY | BLOOD PRESSURE MEASUREMENT (mmHg) | RECOMMENDED MANAGEMENT |
|---|---|---|
| Normal | Systolic less than 120 and diastolic less than 80 |
None |
| Elevated | Systolic between 120 and 129 and diastolic less than 80 |
Estimated ASCVD risk less than 10%: lifestyle changes with blood pressure evaluation in 3 to 6 months |
| Hypertension Stage 1 | Systolic between 130 and 139 or diastolic between 80 and 89 |
Estimated ASCVD risk less than 10%: lifestyle changes with blood pressure evaluation in 3 to 6 months
Estimated ASCVD risk more than 10%: lifestyle changes and anti-hypertensive drug therapy with blood pressure evaluation in 1 month |
| Hypertension Stage 2 | Systolic 140 or higher or diastolic 90 or higher |
Consider 2 anti-hypertension with 2 antihypertensive agents of different classes, coupled with lifestyle changes |
ASCVD=atherosclerotic cardiovascular disease.
Source: Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71(6):e13-e115. Epub November 13, 2017.
TREATING HYPERTENSION
Medications for High Blood Pressure
There are several types of medications used to treat high blood pressure, each working in different ways to help lower blood pressure. Here are the main types:
- Diuretics: Often called “water pills,” diuretics help the body get rid of excess salt and water, which helps lower blood pressure. These are the oldest and cheapest of all blood pressure medications. Examples include hydrochlorothiazide, furosemide and spironolactone.
- Beta blockers: These drugs act on the sympathetic nervous system, which is responsible for the fight-or-flight, adrenaline-fueled response to stress. They also lower your heart rate. Commonly prescribed beta blockers include acebutolol, atenolol, metoprolol and propranolol.
- ACE inhibitors: These drugs help your blood vessels relax and open wider. This improves blood flow and reduces pressure and strain on the heart. Examples include benazepril, captopril and enalapril.
- Angiotensin II receptor blockers (ARBs): Similar to ACE inhibitors, ARBs block the effects of a hormone that narrows blood vessels. They include candesartan, losartan (Cozaar), , telmisartan (Micardis) and eprosartan (Teveten).
- Calcium channel blockers: These medications slow the movement of calcium into the heart and blood vessel walls. This keeps blood vessels open and relaxed and improves the heart’s pumping ability. Examples include amlodipine, diltiazem, felodipine and verapamil.
- Alpha blockers: These drugs reduce the resistance in arteries, relaxing the muscle tone of the vascular walls. Examples include doxazosin and prazosin.
- Alpha-2 receptor agonists: These medications reduce blood pressure by decreasing the activity of the sympathetic nervous system, which is responsible for the “fight or flight,” adrenaline-fueled response to stress. An example is clonidine.
- Vasodilators: These medications directly relax the muscles in the blood vessel walls, which helps widen the vessels and lower blood pressure. Examples include hydralazine and minoxidil.
It’s important to work closely with your healthcare provider to determine the best medication for you. He or she will consider your overall health and any other conditions you may have.
The most common side effects from these medicines are a dry cough, headache, dizziness and fatigue, depending on the medication. A rare side effect with an ACEI or ARB is angioedema, or sudden swelling of the tongue, lips, throat, hands or feet. Call your doctor or 911 immediately if this occurs.
WHOLE PERSON HEALTH AND HYPERTENSION
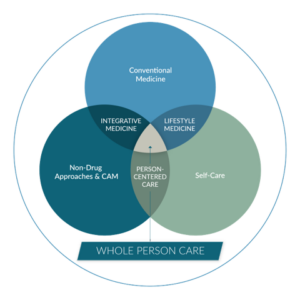
Whether you need medication or not, a whole person health approach can help. This may include diet, exercise and complementary practices such as stress management (Figure 1).
What is Whole Person Health?
 Whole person health is not just about your body – it’s about the health of your mind and spirit, too. Your primary care provider may practice whole person health care, which means they consider everything that goes into making you healthy. What is happening in your life? What are your relationships like? Do you have access to healthful food and clean water? How’s your sense of purpose?
Whole person health is not just about your body – it’s about the health of your mind and spirit, too. Your primary care provider may practice whole person health care, which means they consider everything that goes into making you healthy. What is happening in your life? What are your relationships like? Do you have access to healthful food and clean water? How’s your sense of purpose?
Whole person health care is person-centered and relationship based. Working with a health care provider who understands what is most important to you helps you be as healthy as possible in every way – social, spiritual, emotional, and mental as well as physical. Whole person health also takes your environment into account.
To be effective, whole person health care combines evidence-based conventional medical care – what you probably think of when you think of going to the doctor – with complementary approaches such as acupuncture or meditation and lifestyle medicine, which considers what you eat and drink, how often you get outside, how you are sleeping and more.
Taking a whole person health approach does not necessarily mean giving up your medication. If you have hypertension, medication may be a very important part of staying well. However, a whole person health approach means medication is just one of the ways you treat your high blood pressure. Adding complementary and lifestyle approaches may help you take less medication and eventually, if your doctor agrees, possibly stop taking medication entirely.
A whole health approach to blood pressure management should include the following:
DIET
Hundreds of studies attest to the significant benefits of diet on blood pressure. The Dietary Approaches to Stop Hypertension Eating Plan, sometimes called the DASH diet, is the most tested and practical approach. 16 This eating plan is specifically designed to help people with hypertension. While similar to any form of healthy eating, it also includes a greater emphasis on magnesium and calcium, both of which have been shown to reduce blood pressure, as well as reduce sodium. 17
Using the DASH plan requires no special foods, just meeting daily and weekly nutritional goals. The plan recommends:
- Eating vegetables, fruits and whole grains
- Including fat-free or low-fat dairy products, fish, poultry, beans, nuts and vegetable oils
- Limiting foods that are high in saturated fat, such as fatty meats, full-fat dairy products and tropical oils such as coconut, palm kernel and palm oils
- Limiting sugar-sweetened beverages and sweets
Table 2 highlights what you’d eat if you if you were eating 2,000 calories a day:
TABLE 2: Number of Servings Based on 1800-2000 Calories a Day
| DAILY | |
|---|---|
| Grains | 6-8 |
| Meats, poultry and fish | 6 or less |
| Vegetables | 4-5 |
| Fruit | 4-5 |
| Low-fat or fat-free dairy products | 2-3 |
| Fats and oils | 2-3 |
| Sodium | 1,500 mg – 2,300 mg |
| WEEKLY | |
| Nuts, seeds, dry beans and peas | 4-5 |
| Sweets | 5 or less |
Oh, and cut back on the alcohol. Heavy drinking is a known risk factor for high blood pressure. The American Heart Association recommends no more than one serving daily for women and two for men. 18
STRESS REDUCTION
Stress, both acute and chronic, contributes to high blood pressure by ramping up the sympathetic nervous system, which contributes to the fight-or-flight reaction, including increased heart rate and the release of inflammatory stress hormones such as cortisol. 19 Thus, I recommend relaxation techniques such as those described below.
- Slow, controlled breathing. Simply breathing slowly – defined as six breaths in 30 seconds – can reduce systolic blood pressure by 3.4 mmHg to 3.9 mmHg within minutes compared to just resting. 20 A review of five studies involving 356 people with hypertension found that four out of five demonstrated a significant reduction in blood pressure with slow, controlled breathing. The fifth trial was in people with diabetes, with the researchers concluding that the effects of the diabetes on the autonomic nervous system (which controls body functions such as breathing, heartbeat and digestive processes) likely prevented any benefit. 21 Improving your diabetes with lifestyle changes and medications could restore this responsiveness. Numerous complex mechanisms are believed to contribute to the blood pressure-lowering effects of deep, slow breathing. 20
- You can buy wearable devices that monitor your breathing and remind you to take deep breaths or even start a guided breathing session.
- Meditation. Meditation involves focus and quieting your mind for several minutes or longer. A 2020 review of 14 studies of mindfulness-based interventions found that mindfulness-based stress reduction, mindful breathing and meditation can reduce blood pressure. 22 An analysis of nine trials on meditation found a 4.7 mmHg reduction in systolic blood pressure and a 3.2 mmHg reduction in diastolic blood pressure in people who regularly meditate. 23 It’s not clear just how meditation lowers blood pressure, but it’s likely related to its ability to reduce the physical effects of stress, thus affecting the autonomic nervous system. 20 Talk to your health care provider about using meditation along with medication to lower your blood pressure.
EXERCISE
Put simply, exercise improves hypertension. Indeed, there is just no substitute for physical activity when it comes to blood pressure control. Numerous studies attest to the benefits of regular physical exercise on blood pressure. The benefits appear to be related to the effects exercise has on nitric oxide production, which helps dilate blood vessels, and through the production of anti-oxidants, protects against damaging oxidative stress. Exercise also reduces levels of inflammatory chemicals that can further damage blood vessels.24
The greatest benefits come with aerobic activities, including walking, running, swimming and biking, but isometric exercise designed to build strength, like push-ups, pull-ups and working with weights, can also help. 25 Experts recommend at least 150 minutes of exercise per week for heart health. Talk with your health care provider before starting an exercise program, especially if you have been diagnosed with high blood pressure, take medications for it or have other health conditions. 25
- Tai chi, qi gong, and yoga. There is some evidence that the ancient Chinese martial arts of tai chi and qi gong and the practice of yoga can lead to blood pressure reduction. For yoga, one study found that the breathing and meditation components of yoga practice were as effective at lowering blood pressure as yoga that included physical poses. 26-28 As with meditation and other complementary approaches, talk with your health care provider about using them along with medication. You may be able to use less medication by combining exercise, a breathing practice, or a mindfulness practice with your medically prescribed treatment to lower blood pressure.
OTHER APPROACHES
- Acupuncture. Studies are mixed on acupuncture, but one analysis of two randomized clinical trials comparing real acupuncture to sham acupuncture, both coupled with anti-hypertensive medication, found that acupuncture plus medication was more effective at reducing blood pressure than medication alone, with an average 7.5 mmHg drop in systolic blood pressure and 4.2 mmHg drop in diastolic blood pressure. 29 However, we need more research on this non-drug approach to hypertension. 30
- Massage. Massage may have beneficial effects on blood pressure. However, more studies are needed to learn if massage has a permanent effect on blood pressure. Until we have a definitive answer, talk with your doctor about massage and its effects on blood pressure. 31
What About Taking Supplements?
According to the National Center for Complementary and Integrative Health, no dietary supplement can reproduce the effects of prescription medication to lower blood pressure. So be very cautious about taking supplements based on what you read online or hear from a friend or relative.
Some research suggests that cocoa, garlic, fish oil (omega-3 fatty acids), flaxseed, tea (black or green) probiotics, and the herb roselle (Hibiscus sabdariffa), may be helpful. 32 However, the term to remember is “helpful.” Talk with your doctor or other health care provider before taking any supplements, as they may interact with blood pressure medications or other foods or medications.
Salt Nutrition Facts — What About Salt?
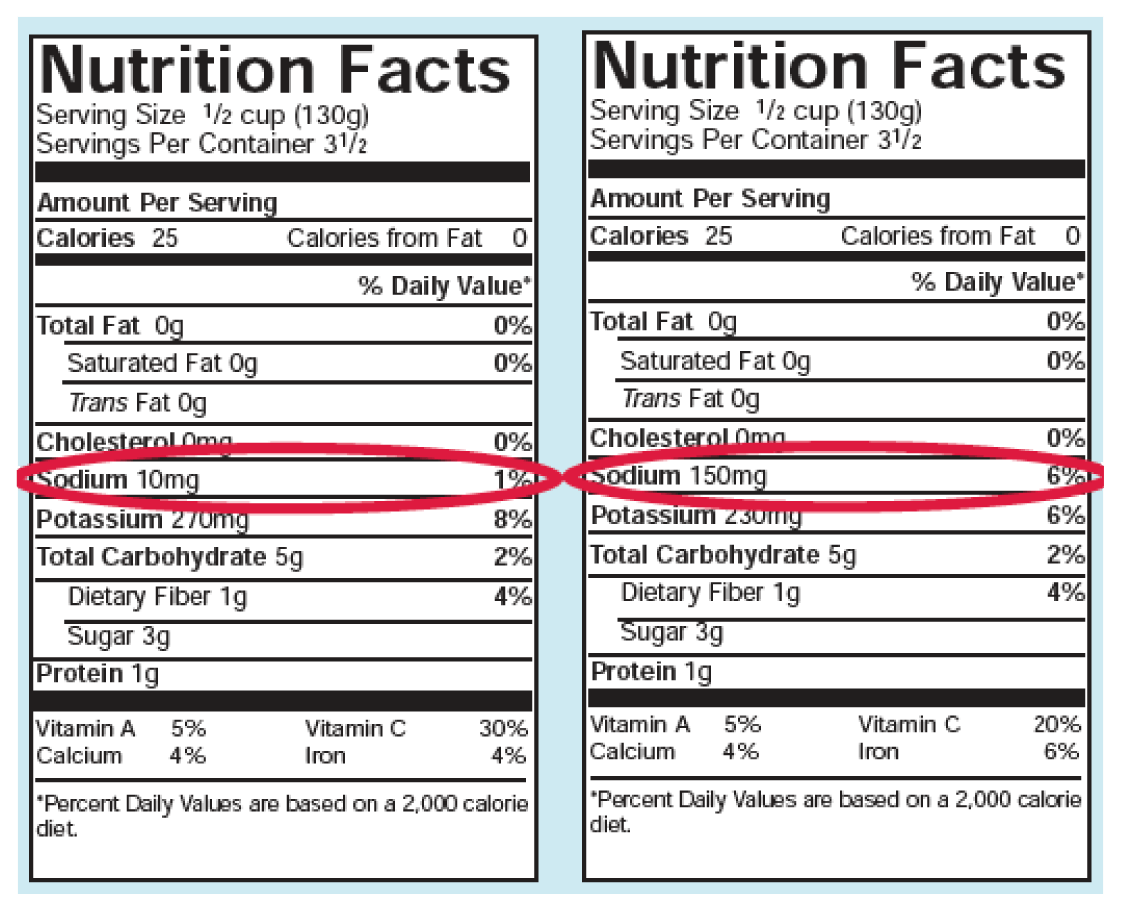
We used to consider sodium the “bad boy” in hypertension and order a salt-free diet. And it’s true that certain people are genetically sensitive to salt. However, the majority of us are not. So should you cut out salt? The research is mixed. But what is clear is that the average American consumes far too much sodium anyway – a daily average of 3,400 milligrams, most of it from processed foods (just take a look at the difference in sodium in low salt versus regular canned tomatoes in Figure 2). Even your breakfast cereal has added salt! So beware of hidden salt. Make sure you read the labels if you have high blood pressure! Reducing sodium consumption can make a big difference for your health. 33
Those whose blood pressure is under control or normal do not need to eliminate salt.
But it’s not just salt…potassium and magnesium matter too!
For those with high blood pressure, making sure you have high levels of potassium and magnesium may be more important than watching your salt. These minerals primarily come from fruits, vegetables, nuts and whole grains, which are the core components of the DASH and Mediterranean diets. Because most Americans don’t eat enough vegetables and fruits, we are low in potassium and magnesium. These minerals all work together in the body to control blood pressure.
THE STORY OF TREVOR
In my book How Healing Works, I tell the story of Trevor. He taught me what can happen when we don’t integrate the various aspects of healing.
Gap In Care
Trevor’s story begins with his diagnosis of hypertension. After college, the former healthy football player had stopped exercising, begun eating whatever he wanted and gained weight. When he finally went in for a long-overdue checkup, his blood pressure was alarmingly high. The doctor prescribed two medications initially, then a third a week later when Trevor’s pressure remained high.
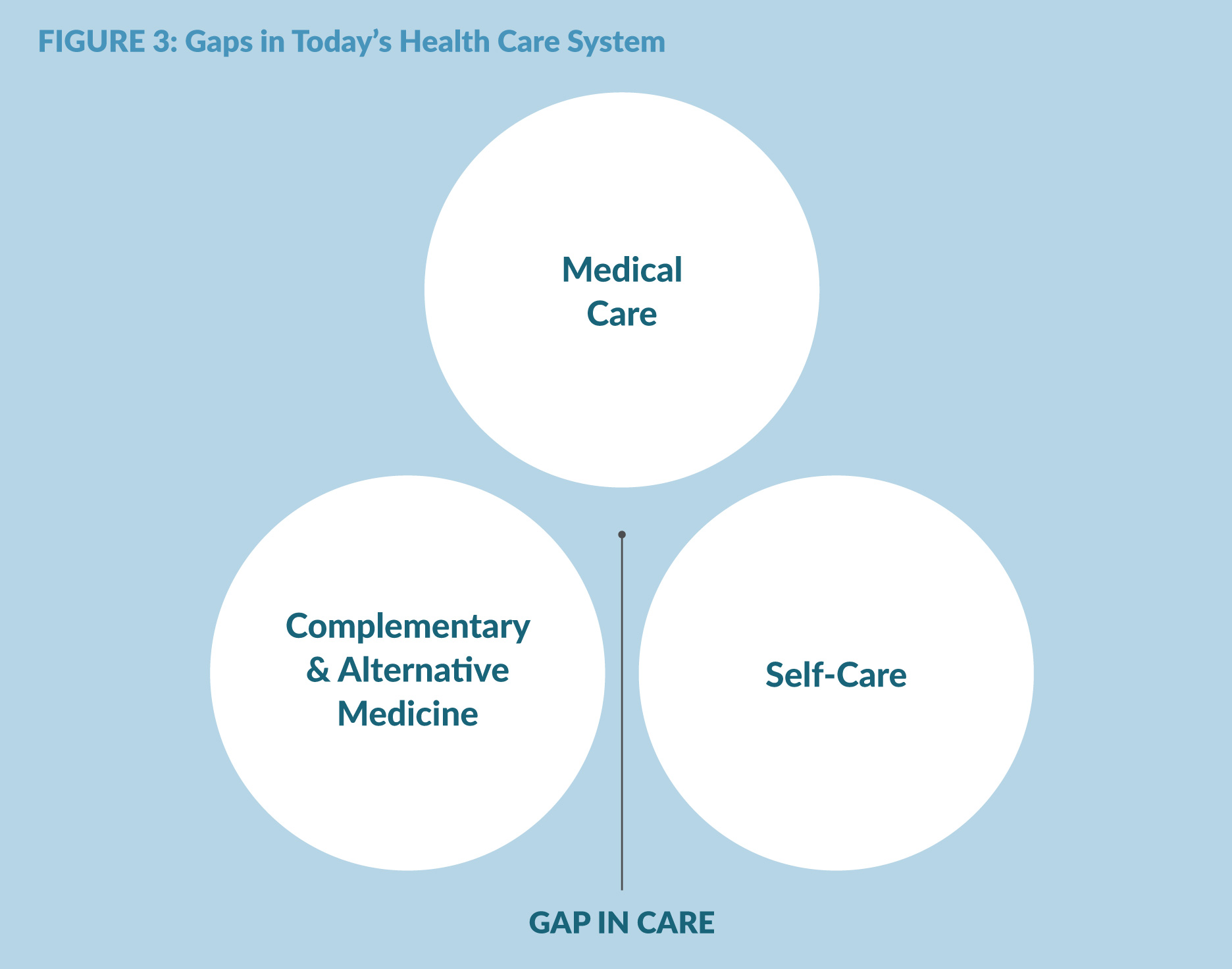
After a few weeks, Trevor’s blood pressure was under control, but he felt terrible. The medications made him tired, interfered with his sexual function and made it hard to sleep. His doctor assured him he would adjust. He also recommended exercise and the DASH diet (but didn’t give Trevor any advice on how to integrate either into his life) and told Trevor he would always need medication. Trevor left his visits alarmed and skeptical. He had felt fine before. Now he felt terrible. Plus, his insurance did not cover the entire cost of drugs.
Where Trevor’s doctor went wrong, however, was in failing to provide empathy and build the trust needed to motivate Trevor to change his life, something current guidelines say should be a standard part of practice. He also didn’t recognize something important about Trevor – a strong preference for “natural” treatments and an inherent optimism that everything would be fine.
A friend recommended a local “natural” practitioner who encouraged Trevor to follow not the DASH diet, but the “rice diet for hypertension.” Trevor, optimistic as always, thought this sounded good and began to work with her. He stopped his medications and started the diet plus supplements. He immediately felt better. After three weeks on the diet and supplements, he checked his blood pressure. It was almost normal. He was back to his old self—or so he thought.
The problem is that unlike the DASH diet, the rice diet was very difficult to follow long-term without substantial professional monitoring and support. In addition, the supplements he was taking did not work to control his hypertension. Since this condition has no signs or symptoms, Trevor thought he was fine. He didn’t see another doctor for ten years—until his feet began to swell.
It turned out that after 10 years of “silent” and poorly treated high blood pressure, he was now in kidney failure. He needed dialysis and was put on the transplant list.
It turned out that after 10 years of “silent” and poorly treated high blood pressure, he was now in kidney failure. He needed dialysis and was put on the transplant list.
Trevor fell into the gap between alternative and conventional medicine and self-care (Figure 3). He needed a whole person health care approach—one that bridged and coordinated the treatments between his biology and the rest of him, between drugs and self-care, between medical treatment and the social and personal determinants of health and between the treatment “agents” and his own “agency”—his inner capacity to heal.
Don’t be like Trevor and fall into the gap between different healing approaches. Understand the limitations of all approaches and the importance of integrating conventional treatments with lifestyle and mind/body approaches. Find a physician you trust, one with empathy, who wants to work with you to integrate evidence-based alternative approaches with drug-based treatments for hypertension.
A good way to start is give your provider a copy of my book How Healing Works and ask them to conduct a HOPE visit as described in the back of the book and on my website healingworksfoundation.org. You will not regret bringing whole person health into your life today.
END NOTES
- Million Hearts. US Department of Health & Human Services. millionhearts.hhs.gov/data-reports/hypertension-prevalence.html. Accessed February 14, 2025.
- World Health Organization. World Hypertension Day 2024. Available at www.who.int/srilanka/news/detail/17-05-2024-world-hypertension-day-2024–measure-your-blood-pressure-accurately–control-it–live-longer. Accessed February 14, 2024.
- American Heart Association. Newsroom. High blood pressure redefined for first time in 14 years: 130 is the new high. Available at newsroom.heart.org/news/highblood-pressure-redefined-for-first-time-in-14-years-130-is-the-new-high. Accessed February 14, 2024.
- Prasantha L Vemu, MD; Eugene Yang, MD, FACC; Joseph Ebinger, MD, FACC. American College of Cardiology. 2023 ESH Hypertension Guideline Update: Bringing us closer together across the pond. Feb 05, 2024. Available at www.acc.org/latest-in-cardiology/articles/2024/02/05/11/43/2023-esh-hypertensionguideline-update. Accessed February 14, 2025.
- Lim SS, Vos T, Flaxman AD, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2224-2260.
- U.S. Centers for Disease Control and Prevention. High blood pressure facts. Updated January 8, 2025. Available at www.cdc.gov/high-blood-pressure/data-research/facts-stats/index.html. Accessed February 24, 2025.
- National Center for Health Statistics. Multiple Cause of Death 2018–2022 on CDC WONDER Database. Accessed February 18, 2025. wonder.cdc.gov/mcd.html
- Centers for Disease Control and Prevention. Hypertension cascade: hypertension prevalence, treatment and control estimates among US adults aged 18 years and older applying the criteria from the American College of Cardiology and American Heart Association’s 2017 Hypertension Guideline—NHANES 2017–March 2020. Published 2023. Accessed February 18, 2025. Available at millionhearts.hhs.gov/datareports/hypertension-prevalence.html
- American Heart Association. Heart disease and stroke could affect at least 60% of adults in U.S. by 2050. June 4, 2024. Available at www.heart.org/en/news/2024/06/04/heart-disease-and-strokecould-affect-at-least-60-percent-of-adults-in-us-by-2050?form=MG0AV3. Accessed February 18, 2025.
- Vasan RS, Beiser A, Seshadri S, et al. Residual lifetime risk for developing hypertension in middle-aged women and men: The Framingham Heart Study. JAMA. 2002;287(8):1003–1010. doi:10.1001/jama.287.8.1003
- US Centers for Disease Control. High blood pressure risk factors. December 13, 2024. Available at www.cdc.gov/high-blood-pressure/risk-factors/index.html. Accessed February 18, 2025.
- National Institute on Aging. High blood pressure and older adults. Content reviewed October 1, 2022. Available at www.nia.nih.gov/health/high-bloodpressure/high-blood-pressure-and-older-adults. Accessed February 18, 2025.
- Hall JE, do Carmo JM, da Silva AA, Wang Z, Hall ME. Obesity-induced hypertension: interaction of neurohumoral and renal mechanisms. Circ Res. 2015;116(6):991-1006.
- American Heart Association. Home blood pressure monitoring. Last reviewed May 20, 2024. Available at www.heart.org/en/health-topics/high-blood-pressure/understanding-blood-pressure-readings/monitoringyour-blood-pressure-at-home. Accessed February 18, 2025.
- Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines. Hypertension. 2018;71(6):e13-e115. Epub November 13, 2017.
- National Heart, Lung, and Blood Institute. DASH Eating Plan. Last updated January 10, 2025. Available at www.nhlbi.nih.gov/education/dash-eating-plan. Accessed February 24, 2025.
- Saneei P, Salehi-Abargouei A, Esmaillzadeh A, Azadbakht L. Influence of Dietary Approaches to Stop Hypertension (DASH) diet on blood pressure: a systematic review and meta-analysis on randomized controlled trials. NutrMetab Cardiovasc Dis. 2014;24(12):1253-1261.
- American Heart Association. Limiting alcohol to manage high blood pressure. May 7, 2025. Available at www.heart.org/en/health-topics/high-blood-pressure/changes-you-can-make-to-manage-high-bloodpressure/limiting-alcohol-to-manage-high-bloodpressure. Accessed February 24, 2025.
- Joyner MJ, Charkoudian N, Wallin BG. Sympathetic nervous system and blood pressure in humans individualized patterns of regulation and their implications. Hypertension. 2010;56(1):10-16.
- Brook RD, Appel LJ, Rubenfire M, et al. Beyond medications and diet: alternative approaches to lowering blood pressure: a scientific statement from the American Heart Association. Hypertension. 2013;61(6):1360-1383.
- Parati G, Carretta R. Device-guided slow breathing as a non-pharmacological approach to antihypertensive treatment: efficacy, problems and perspectives. J Hypertens. 2007;25(1):57-61.
- Intarakamhang U, Macaskill A, Prasittichok P. Mindfulness interventions reduce blood pressure in patients with non-communicable diseases: A systematic review and meta-analysis. Heliyon. 2020 Apr 28;6(4):e03834. doi: 10.1016/j.heliyon.2020.e03834. PMID: 32373739; PMCID: PMC7191601.
- Anderson JW, Liu C, Kryscio RJ. Blood pressure response to transcendental meditation: a meta-analysis. Am J Hypertens. 2008;21(3):310-316.
- Korsager Larsen M, Matchkov VV. Hypertension and physical exercise: the role of oxidative stress. Medicina (Kaunas). 2016;52(1):19-27.
- American Heart Association. Getting active to control high blood pressure. May 22, 2024. Available at www.heart.org/en/health-topics/high-blood-pressure/changes-you-can-make-to-manage-high-bloodpressure/getting-active-to-control-high-blood-pressure. Accessed February 24, 2025.
- Zhong D, Li J, Yang H, Li Y, Huang Y, Xiao Q, Liu T, Jin R. Tai chi for essential hypertension: a systematic review of randomized controlled trials. Curr Hypertens Rep. 2020 Mar 2;22(3):25. doi: 10.1007/s11906-020-1031-y. PMID: 32124064.
- Liu D, Yi L, Sheng M, Wang G, Zou Y. The efficacy of tai chi and qigong exercises on blood pressure and blood levels of nitric oxide and endothelin-1 in patients with essential hypertension: A systematic review and metaanalysis of randomized controlled trials. Evid Based Complement Alternat Med. 2020 Jul 30;2020:3267971.doi: 10.1155/2020/3267971. PMID: 32802122;PMCID: PMC7414352.
- Cramer H, Sellin C, Schumann D, Dobos G. Yoga in arterial hypertension. Dtsch Arztebl Int. 2018 Dec 14;115(50):833-839. doi: 10.3238/arztebl.2018.0833. PMID: 30722837; PMCID: PMC6375068.
- Zhao XF, Hu HT, Li JS, et al. Is acupuncture effective for hypertension? A systematic review and meta-analysis. PLoS One. 2015;10(7):e0127019.
- Fan M, Dai G, Li R, Wu X. Efficacy of acupuncture in the treatment of essential hypertension: an overview of systematic reviews and meta-analyses. Cardiovasc Ther. 2023 Apr 18;2023:2722727. doi:10.1155/2023/2722727. PMID: 37113506; PMCID:
PMC10129421. - Vijayakumar V, Boopalan D, Ravi P, Chidambaram Y, Anandhan A, Muthupandi P, Shanmugam P, Kuppusamy M, Karuppasamy G. Effect of massage on blood pressure in patients with hypertension: A metaanalysis. J Bodyw Mov Ther. 2024 Jan;37:109-114. doi: 10.1016/j.jbmt.2023.11.028. Epub 2023 Nov 22. PMID: 38432790.
- National Center for Complementary and Integrative Health. Hypertension (high blood pressure). July 2018. Available at www.nccih.nih.gov/health/hypertensionhigh-blood-pressure. Accessed February 24, 2025.
- Doctrow, B. Lower sodium could reduce blood pressure in most people. NIH Research Matters. December 5, 2023. Available at www.nih.gov/news-events/nihresearch-matters/lower-sodium-could-reduce-bloodpressure-most-people. Accessed February 24, 2025.
Topics: Behavior & Lifestyle | Blood Pressure | Chronic Disease | Diet | Exercise | Herbs & Supplements | Hypertension | Integrative Health | Nutrition | Relaxation | Self-Care | Stress | Stress Management | Weight Loss
