
Your Healing Journey: A Patient’s Guide to Integrative Breast Cancer Care
Relieve breast cancer symptoms and reduce treatment side effects with evidence-informed self-care, complementary and lifestyle approaches used with conventional cancer treatments
LETTER FROM DR. WAYNE JONAS
Dear Friend,
When my wife, Susan, was diagnosed with breast cancer for the second time after 26 years, we both knew that we would have to tap deeply into her healing capacity.
A MEANINGFUL LIFE
Susan was only 35, and the mother of three young children, when she discovered she had breast cancer for the first time. While I was looking for cures, Susan wanted to weigh the treatment recommendations against her values and goals for a meaningful life.
One of the first things Susan did was to reach out to family and friends and find support for her children. This support network allowed her to undergo intensive chemotherapy and recover rather rapidly, but not without some long-term residual problems including increased weight, early onset of menopause, some cognitive impact (called chemo brain), lymphedema and mild damage to her nerves, which causes numbness and tingling in her fingers and toes.
Social support from family and friends helped Susan get through and recover from intensive chemotherapy.
Back then, oncologists did not make recommendations on integrating a healthy lifestyle, including social support or complementary medicine, with conventional breast cancer care. Had Susan been encouraged to exercise, eat healthy food and engage in major stress management, some of her long-term problems could have been reduced.
THE NEED FOR INTEGRATIVE BREAST CANCER CARE
Twenty-five years later, our three-month-old grandson helped discover Susan’s second breast cancer. When our daughter-in-law had complications after his birth, Susan volunteered to help care for the baby. One day she noticed her breast was sore when she held him. That turned out to be another type of breast cancer.
Things were somewhat different this time. Lectures on nutrition, yoga classes and support groups for cancer patients are now common. Doctors acknowledge the role of healthy behavior in surviving cancer. But most doctors aren’t trained in how to use behavioral or complementary approaches to help cancer patients. Advances in the science of healthy behavior are still not integrated into the delivery of cancer care.
Our oncologist, one of the best in the region, did not know about the Society for Integrative Oncology, where mainstream oncologists together with experts in complementary medicine explore the integration of healing practices with cure-focused treatments in cancer.
A HEALING SPACE
Treatment for Susan’s second breast cancer involved three types of chemotherapy and a double mastectomy. Susan’s focus on a meaningful life, and the healing space she created and filled with social support, were essential to her healing journey.
Susan turned our bedroom into a safe, soothing place to rest and bring our grandbaby into. She had the walls painted a light blue-grey. They were bare except for one wall—where Susan hung an abstract painted by a good friend that almost blended into the wall. White opaque curtains covered the windows. We bought a new and more comfortable bed and placed it in front of the French doors, where natural, indirect light bathed the room in a soft glow. The room looked as if it was ethereal, simple, uncluttered and peaceful.
Caring for our grandson, even when Susan needed help to do this, gave meaning to her life. In the corner of the bedroom, Susan set up a play area for the baby and some chairs where others could sit when our grandchild was in the room.
Healing spaces and healing relationships stimulate recovery.
After surgery, relatives, friends and neighbors came to sit with Susan while she recovered. Some cooked, cleaned and helped with the grandbaby. Others simply offered their caring and their presence.
Our youngest daughter, a singer and a teacher, recorded a special set of songs for each phase of Susan’s recovery, bringing humor and laughter into the house. This is a complementary approach for cancer called music therapy.
YOUR GUIDE TO INTEGRATIVE HEALING
Susan and I want to help other women with breast and other cancers heal.
Lifestyle approaches such as social support, healthy eating and exercise and complementary approaches such as yoga, acupuncture and music therapy are part of integrative breast cancer care. These approaches can:
- Activate your ability to heal
- Help you feel better physically and emotionally
This guide covers complementary and lifestyle approaches that can be used along with conventional breast cancer treatments. This is called integrative breast cancer care.
I hope that you’ll find this guide useful on your healing journey.
Be well.
Wayne Jonas, MD
SAFE AND EFFECTIVE WAYS TO FEEL BETTER
Hearing the words “you have breast cancer” is overwhelming. You probably didn’t remember anything the doctor said after the word “cancer.” Telling your friends and family made you realize how scared you are.
You want to do everything that you can to get well. You need to feel better and stay strong during and after treatment. And you need to protect yourself from the effects of fear.
Along with conventional medical care, complementary and lifestyle approaches can help you in your healing journey. These approaches can help relieve many breast cancer symptoms and treatment side effects. But what can help you and what might hurt you? Some things don’t work. Others can interfere with your conventional cancer treatment. Others help.
“Patients often seek information about complementary therapies on the Internet and/or receive information from well-meaning friends and family. Unfortunately, there is a lot of inaccurate information out there. And many times we don’t have data to let us know if products or approaches are safe and effective.”
AN INTEGRATIVE APPROACH TO BREAST CANCER CARE
This guide will help you find safe and effective complementary and lifestyle approaches that you can use along with conventional cancer treatments. This is called integrative breast cancer care, which can:
- Minimize anxiety, stress and depression
- Relieve other cancer symptoms and treatment side effects
- Boost your overall sense of wellbeing
Always talk to your cancer care team before using complementary and lifestyle approaches. “We can make sure you get the information that will help you safely use integrative therapies during and after treatment,” says Gabriel Lopez, MD, medical director of the Integrative Medicine Center at the MD Anderson Cancer Center. Dr. Lopez is a medical oncologist and assistant professor at the University of Texas MD Anderson Cancer Center.
The content in this guide is evidence informed, based on the best available information at the time of publication. Resources used include expert opinion, clinical practice guidelines and research published in peer-reviewed journals. Integrative breast cancer care helped Jenny Leyh. It can help you too.
What helps with anxiety and stress?
Just a few minutes of meditation—5 to 20 minutes a day—can help you feel calmer and more relaxed.
Integrative Approach Empowers Jenny Leyh to Heal
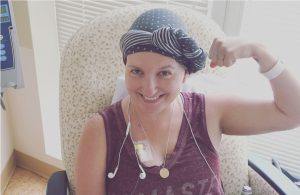 Jenny Leyh was 33 and in the third trimester of her pregnancy when she was diagnosed with breast cancer in May 2016. “I still vividly recall hearing the words ‘you have cancer.’ After I hung up the phone, I sat in silence not knowing what to do next,” says Leyh, who lives in Baltimore, Md.
Jenny Leyh was 33 and in the third trimester of her pregnancy when she was diagnosed with breast cancer in May 2016. “I still vividly recall hearing the words ‘you have cancer.’ After I hung up the phone, I sat in silence not knowing what to do next,” says Leyh, who lives in Baltimore, Md.
“After the initial shock wore off, I was determined to fight the cancer with everything I had,” she says. That’s exactly what Leyh did. Along with her conventional cancer treatments, she used acupuncture, exercise, healthy eating, meditation and yoga to stay strong during treatment and relieve her anxiety and treatment side effects.
An Aggressive Breast Cancer
Leyh had triple negative breast cancer, stage IIb, with a grade III tumor. This subtype of breast cancer is extremely aggressive, and Leyh needed to start treatment right away. Doctors at Johns Hopkins Medicine recommended chemotherapy (chemo) before surgery to help combat the cancer without harming Leyh’s baby. Her medical oncologist worked closely with her OB/GYN in developing the cancer treatment plan and monitoring Leyh’s daughter until she was safely born in June 2016.
Chemo Causes Unbearable Pain
Over a year, Leyh completed 16 rounds of chemo, followed by a bilateral mastectomy with tissue expanders and then radiation therapy. She didn’t have the common chemo side effects of nausea, vomiting and diarrhea. But as each round of chemo shrank Leyh’s tumor, the harsh treatment also wrought havoc on her body in other ways. She had joint pain, debilitating fatigue, bleeding hemorrhoids, tender fingernails and toenails and a general flu-like feeling. Each round of chemo made her feel worse.
“The joint pain and fatigue were particularly persistent and became increasingly unbearable,” says Leyh. The pain started mildly in Leyh’s ankles, spreading first to her knees and then to her hips and wrists and becoming more intense.
“When I got up after sitting for any length of time, my ankles stiffened. My feet felt tender and any amount of pressure caused me to limp in pain. My wrists were often sore and I had trouble rotating them into particular positions.”
Yoga and Acupuncture Relieve Pain
When Leyh had difficultly lifting her daughter, she knew she had to take action. Instead of the pain meds her doctor prescribed, which would cause more side effects, she turned to gentle yoga and acupuncture.
“Yoga is a healthy outlet for pain management. The deliberate movements helped to ease the pain in my hips, ankles and feet and also gave me a boost of energy,” says Leyh who had been practicing yoga for years. She also used acupuncture, which helped ease her pain.
Exercise and Healthy Eating Improve Wellbeing and Boost Energy
Getting light exercise regularly and eating healthy also improved Leyh’s overall wellbeing and helped her reduce the negative thoughts that come with battling cancer. She also knew that maintaining a healthy weight and being physically active could help her lower the risk that her breast cancer would come back or that she’d develop another type of cancer.
Along with yoga, Leyh stayed active by taking light walks. The exercise relieved her joint pain.
Leyh ate a healthy, mostly vegetarian diet. “I had been raised a vegetarian, but I wouldn’t say I was a particularly healthy eater. When I was diagnosed I became more selective about what I was eating. I bought a juicer and began cooking meals made from whole foods and experimented with spices. This helped boost my immune system and increase my energy level,” she says.
Now, Leyh sees food as more than just nourishment for her body. “Food is also medicine, and it’s even a preventative measure,” she says.
A Positive Attitude after Treatment
Doctors told Leyh she was cancer free in April 2017. But like many cancer survivors, she still had late effects from her treatments and was worried about her cancer coming back.
“I was physically beat up and emotionally struggling, and I felt almost as lost as I had when I was first diagnosed,” she says. After a few months of feeling unable to shake the anxiety, Leyh went on a low dose antidepressant, began to see a therapist, started meditating and continued practicing yoga and getting acupuncture.
“Yoga is an amazing outlet. I had practiced for many years but when I was diagnosed with breast cancer, it was something I turned to for a physical challenge and it left me feeling at peace. My practice went from once a week to something that I not only wanted, but I needed to do on a daily basis. The combination of low-impact exercise, meditation, therapy and the antidepressant helped me through some dark times,” says Leyh.
“Self-care is so important when you are going through a difficult period. Taking some time for yourself and doing things that help you to relax can really go a long way,” she says.
Find What Works for You
Leyh used a mix of integrative health approaches that helped in her fight against breast cancer. You can too. “There isn’t a one-size-fits-all approach to integrative breast cancer care,” she says. “You have to find what’s most meaningful and effective for you.”
The traditional care for breast cancer is almost written in stone. It often involves surgery, chemo, or radiation or some combination of these treatments. But going through cancer is more than just the treatments. The side effects are the real challenge and everyone responds differently to the drugs. “I didn’t want to just medicate the problems away,” says Leyh. “Integrative therapies helped me to be proactive in my treatment plan.”
Leyh’s daughter, Chloë, is now two years old. The pair have been enjoying a summer filled with trips to the playground and cooling off under the sprinkler in the backyard. Leyh also taught Chloë how to ride a tricycle. While Leyh still struggles with the physical and emotional wounds of her cancer care, it gets better with each day.
“My breast cancer diagnosis was devastating for both me and my family,” says Leyh. “But it has also taught me so much about myself and what I am capable of. I truly believe that ‘what doesn’t kill you makes you stronger.’ Breast cancer knocked me down and left a few scars on my body. But I got up stronger than I was before. My family, my medical team, my yoga instructor, my therapist, my acupuncturist, my ‘breasties;’ all of those factors contributed to my overall care and helped me to get well again.”
COMPLEMENTARY AND LIFESTYLE APPROACHES
Complementary approaches are any medical system, practice, or product that is not part of conventional medicine. Lifestyle approaches are healthy, evidence-based self-care and behavioral approaches to enhance health and healing. Both of these should be used along with, and never instead of, conventional cancer care.
Other key terms related to integrative breast cancer care and other treatments for breast cancer are:
- Integrative medicine, the coordinated use of evidence-based complementary practices and conventional medicine
- Integrative oncology, the use of complementary and integrative therapies along with conventional cancer care
- Alternative medicine, which is used instead of conventional medicine. Alternative medicine is any medical system, practice or product that is not part of conventional medicine. Women with breast cancer should never use alternative medicine
If it’s natural, how can it hurt me?
Many people think that natural products like dietary supplements are safe. But some dietary supplements can interfere with your cancer treatment. St. John’s Wort, for example, makes chemo less effective and worsens skin problems from radiation therapy.
Men get breast cancer too
99 percent of breast cancer occurs in women, but men also get breast cancer. The information about complementary and lifestyle approaches in this guide is applicable to men with breast cancer too.
Definition of Integrative Oncology
Here is the full definition of integrative oncology:
“Integrative oncology is a patient-centered, evidence-informed field of cancer care that utilizes mind and body practices, natural products and/or lifestyle modifications from different traditions alongside conventional cancer treatments. Integrative oncology aims to optimize health, quality of life and clinical outcomes across the cancer care continuum and to empower people to prevent cancer and become active participants before, during and beyond cancer treatment.”
Source: “A Comprehensive Definition for Integrative Oncology,” JNCI Monographs, Volume 2017, Issue 52, 1 November 2017
We use the term “integrative breast cancer care” to describe integrative oncology for women with breast cancer
How can I feel better during chemo?
The ancient Chinese practice of acupuncture, healthy eating and exercise all help relieve nausea and vomiting from chemo. Ginger can help a little too.
What should I eat?
The Mediterranean diet may help lower the risk of dying from breast cancer and prevent recurrence. Fish, vegetables, legumes, whole grains, fruits, and extra virgin olive oil are the main foods in the Mediterranean diet. You can also have some wine and a little red meat.
When is it not okay to exercise?
Moderate exercise can boost your energy and mood and help relieve some symptoms of cancer and side effects of treatment. But don’t exercise if you have:
- Pain, nausea/vomiting or any other symptom that won’t go away and worries you
- Abnormal levels of sodium, potassium and other minerals from vomiting or diarrhea
- A low red blood cell count (anemia)
Am I weak if I ask for help?
Joining a support group or asking family and friends for help doesn’t mean you’re weak. No matter how strong you are, social support can empower you to fight your cancer.
Common Symptoms and Side Effects
Complementary and lifestyle approaches can help with many breast cancer symptoms and treatment side effects, including:
- Anxiety and stress
- Eating problems
- Fatigue
- Hot flashes
- Mood problems and depression
- Nausea and vomiting from chemotherapy
- Poor quality of life
- Pain
- Sleep problems
Complementary Approaches
In this guide we cover these complementary approaches:
- Acupressure
- Acupuncture
- Massage therapy
- Meditation
- Music therapy
- Relaxation techniques
- Yoga
Lifestyle Approaches
In this guide we cover these lifestyle approaches:
- Healthy eating
- Dietary supplements
- Exercise and physical activity
- Social support
HOW INTEGRATIVE BREAST CANCER CARE WORKS
Now we’re going to tell you more about how integrative breast cancer care works, and the evidence behind complementary and lifestyle approaches.
On page 17, we highlight common symptoms and side effects and the approaches that can help.
After that, we describe each complementary and lifestyle approach. We include the evidence for each approach, along with recommendations and tips.
How Do I Find Integrative Breast Cancer Care?
Many leading cancer centers offer integrative oncology or integrative medicine services or programs. National Cancer Institute- (NCI-) Designated Cancer Centers provide cutting-edge cancer treatments. Many of them offer integrative oncology or medicine services or related programs. There are NCI cancer centers in 36 states and the District of Columbia.
Find NCI cancer centers in your state or region. Then visit their websites to see if they offer integrative oncology or medicine.
Adding Integrative Care to Your Treatment Plan
If your cancer center doesn’t offer integrative oncology or medicine, talk to your doctor about how you can add complementary and lifestyle approaches to your treatment plan.
Share with your doctor:
- The Society for Integrative Oncology guidelines on integrative treatment during and after breast cancer treatment, endorsed by the American Society of Clinical Oncology
- Recommendations on healthy eating and exercise and physical activity in this guide
Integrative Medicine at MD Anderson Cancer Center

At the first visit to the Integrative Medicine Center at MD Anderson Cancer Center (MD Anderson), women with breast cancer often make a confession: They don’t really know why they’re there. But once they see how integrative therapies help them deal with stress and anxiety and improve their wellbeing, they’re glad they followed their oncologist’s advice to make the appointment.
The Customized Integrative Care Plan
Women with breast cancer use more integrative therapies than other cancer patients. “We work with each patient to develop an integrative care plan based on her interests and where she is on her cancer care journey,” says Dr. Lopez, who is one of three integrative medicine doctors at MD Anderson. The integrative care plan is developed in consultation with the patient’s primary cancer team as part of a comprehensive approach to cancer care.
An integrative oncology consultation with Dr. Lopez or another of the center’s doctors or nurse practitioners is the first step. The consultation includes a thorough assessment of symptoms and side effects, nutrition, physical activity, sleep quality and mood. The provider also asks the patient about her top two interests related to integrative medicine.
Safe and Effective Integrative Approaches
Each plan includes only safe and effective integrative approaches for cancer, such as:
- Acupuncture
- Exercise and physical activity consultations
- Health psychology
- Meditation
- Music therapy
- Nutrition consultations
- Oncology massage
All services are provided at MD Anderson, and the Integrative Medicine Center has licensed clinical psychologists, acupuncturists and massage therapists. Along with consultations and one-on-one services, the center offers a variety of classes and programs, including:
- Physical classes such as “Get Moving” (a blend of yoga, dance and martial arts), “Shape-Up Circuit” (stations with different exercises) and tai chi
- Mind and body classes, including “Yoga for Health,” “Meditation for Health,” “Meditation and Daily Life” and qigong
- Laughter for Health Yoga, Meditation for Daily Life and Mindful Meditation
- Social classes such as “Cooking for Optimal Health”
The integrative care plan is monitored and adjusted during follow-up visits. “We re-assess the patient’s symptoms, how successful the integrative therapies are in meeting the patient’s goals and where the patient is in her cancer treatment,” says Dr. Lopez. Along with visits to Dr. Lopez or another provider, staff members providing integrative services also monitor care.
Integrative Therapies Based on the Breast Cancer Journey
The right integrative therapies usually depend on the woman’s place in the breast cancer journey. “Sometimes we see patients at diagnosis and the next steps are not clear. We can provide education about the role of integrative medicine in supporting their health along the way,” says Dr. Lopez.
If a patient is having treatment, the recommended integrative therapies will focus on relieving symptoms or side effects. For example, Dr. Lopez may recommend acupuncture for relief of nausea and vomiting from chemo or an exercise consultation to develop a plan to conserve energy when a woman experiences fatigue during radiation therapy. Recent evidence suggests that interventions such as acupuncture may be helpful in providing relief for
joint pain or hot flashes from hormone therapy after treatment.
Communication and Coordination with the Cancer Care Team
Having all integrative therapies and services available at MD Anderson makes it easy for the patient’s primary cancer team and the integrative medicine staff to stay updated on what’s happening with each patient. Like medical treatments, the integrative oncology consultation and all integrative services provided become part of the electronic
medical record.
MD Anderson is the #1 cancer center in the United States, according to U.S. News and World Report (2018-2019), and an NCI-Designated Comprehensive Cancer Center.
Collaborate to Develop Your Personal Plan
An integrative oncology or medicine doctor will partner with you and members of your cancer care team to create a safe and effective integrative breast cancer care plan for you. The plan will include specific complementary and lifestyle approaches. Usually, the integrative oncology or medicine doctor will recommend services, programs and providers at or outside of your cancer center.
Integrative Medicine at the Seattle Cancer Care Alliance

“Integrative medicine therapies and practices can be empowering, therapeutic tools to help relieve cancer- and treatment-related side effects and improve overall wellness and quality of life during any stage of treatment and survivorship,” says Dr. Greenlee.
Education, Training, Counseling and Services
The first integrative medicine appointment at the Seattle Cancer Care Alliance starts with discussing the patient’s health and lifestyle, and her/his health and wellness goals. Then the integrative medicine provider and the patient work together to design an individualized plan to help the patient achieve them.
Integrative medicine visits and plans can include:
- Education on dietary supplements and other natural products
- Training in mind and body therapies such as progressive muscle relaxation, relaxation breath work, guided imagery, mindfulness-based stress reduction, mindful eating and self-hypnosis
- Lifestyle counseling, including nutrition, weight management, physical activity and sleep
- Acupuncture
- Massage therapy
- Yoga
The Seattle Cancer Care Alliance is the clinical care partner for the Fred Hutchinson Cancer Research Center and the University of Washington Consortium, an NCI-Designated Comprehensive Cancer Center.
“So much of what it means to heal has to do with coming up with an individualized plan– something meaningful and doable for the patient,” says Wayne Jonas, MD. “While undergoing cancer treatment, healing and curing have to come together. Through integrative health a patient can be empowered to activate their ability to truly heal.” Dr. Jonas is a practicing family physician, an expert in integrative health care delivery and a widely-published scientific investigator.
Finding Providers of Complementary Approaches
If your cancer center can’t recommend a provider for a complementary approach you’re considering, the Society for Integrative Oncology has information about training and licensing for providers of:
- Acupuncture
- Hypnosis
- Massage therapy
- Meditation
- Music therapy
- Relaxation and stress management techniques
- Yoga
Table 2 of the society’s breast cancer guidelines also highlights professional societies and organizations where you can learn more about providers for each complementary approach.
Look for Experience with Cancer and Collaboration
“Ideally, we want patients to work with a provider who has experience working with cancer patients and a track record of collaborating with conventional providers, and who is regularly monitoring for problems,” says Dr. Greenlee.
Source: Society for Integrative Oncology, “Clinical practice guidelines on the evidence-based use of integrative therapies during and after breast cancer treatment.”
Always Collaborate with Your Cancer Care Team
Integrative breast cancer care means using complementary and lifestyle approaches along with conventional cancer treatments. Complementary and lifestyle approaches should never be used instead of conventional cancer treatments.
Always talk to your doctor and other members of your cancer care team about any complementary and lifestyle approaches you’re using or thinking about using. You can use social support on your own.
“We want to make sure there’s evidence suggesting the approaches being chosen are effective for managing your symptom, side effect or health goal, and that there are no interactions with chemo, radiation or healing from surgery,” says Dr. Greenlee.
Your doctor can also help you make sure that the complementary and lifestyle approaches you want to use work together and with your conventional cancer treatments. He or she can monitor the effectiveness of complementary and lifestyle approaches and suggest other approaches if something’s not working.
EVIDENCE-INFORMED INTEGRATIVE APPROACHES
Evidence from research is needed to know whether a complementary or lifestyle approach works and whether it could interfere with your conventional breast cancer treatment or harm you.
“There are a lot of therapies and approaches out there that are not effective, and some that are harmful,” says Dr. Greenlee. “We want patients and clinicians to use evidence to make informed decisions about what to use and what not to use.”
CURRENT EVIDENCE ANSWERS SOME QUESTIONS
Evidence about the safety and effectiveness of complementary and lifestyle approaches for cancer is growing. But there are still many questions to be answered.
Integrative oncology departments or programs of NCI-Designated Cancer Centers usually only use complementary and lifestyle approaches that have some credible evidence showing they can help with cancer symptoms and treatment side effects.
QUALITY OF THE EVIDENCE VARIES
The information in this guide is evidence informed. This means that it is based on scientific research or information about the use of integrative approaches in treating breast cancer or cancer in general. But it is not medical advice and it doesn’t replace the advice you get from your cancer care team.
Mind and Body Practices and Lifestyle Approaches Work
When choosing complementary and lifestyle approaches, think about the benefit/risk ratio. “A lot of people hope a dietary supplement or natural product will be a magic bullet,” says Dr. Greenlee. “Unfortunately, we don’t have a lot of data that dietary supplements are effective.”
But evidence is very strong for mind and body practices and healthy eating and exercise and physical activity. “We do have a lot of data suggesting that mind and body therapies can be quite effective at managing some forms of
depression, anxiety and fatigue,” she says.
There is also strong evidence that healthy eating and exercise and physical activity help women with breast cancer feel better during and after treatment.
“If you’re choosing between things you can do, focus on mind and body practices and diet/physical activity,” says Dr. Greenlee.
The quality of the evidence for different complementary and lifestyle approaches varies. Few of these approaches have the type of rigorous evidence that is used to evaluate conventional medical treatments. For people with cancer, there is:
- Good evidence that some approaches are safe and effective
- Good evidence that some approaches are harmful or don’t work
- Too little evidence on some approaches to know whether they are safe and effective
Finding Trustworthy Information Online
“It’s always good to have a healthy skepticism about what’s out there. Stay safe,” says Dr. Lopez.
You can find useful, trustworthy information online about complementary and lifestyle approaches for cancer. But there’s also a lot of information that’s inaccurate, misleading, fraudulent or not informed by evidence.
Work with your doctor to choose the complementary and lifestyle approaches that will be safe and effective for you.
Guides to Trustworthy Information
These guides can help you find credible sources of information and evaluate what you read online:
- Don’t Believe Everything You Read on the Internet, from the Society for Integrative Oncology
- Finding and Evaluating Online Resources, from the National Center for Complementary and Integrative Health
EVIDENCE USED IN THIS GUIDE
Much of the evidence in this guide comes from the Society for Integrative Oncology’s “Clinical practice guidelines on the evidence-based use of integrative therapies during and after breast cancer treatment.”
Other key sources of evidence are:
- The American Cancer Society, which funds and conducts research, shares expert information, supports patients and spreads the word about preventing cancer
- The American Institute for Cancer Research, which funds cutting-edge research and gives people practical tools and information to help them prevent—and survive—cancer
- The LIVESTRONG Foundation, which unites, inspires and empowers people affected by cancer and provides free cancer support services
- Savor Health™, which provides cancer nutrition expertise to make the lives of people with cancer easier
Evidence from the Society for Integrative Oncology and some other evidence is specific to breast cancer. Some of the evidence is about cancer in general.
Evidence from the Society for Integrative Oncology
In 2017, the Society for Integrative Oncology published guidelines for doctors and patients on integrative therapies (called complementary and lifestyle approaches in this guide) during and after breast cancer treatment. Experts reviewed scientific evidence from studies about many complementary approaches and categorized each approach based on the available evidence, benefits versus risks, practicality and value.
Most lifestyle approaches (diet, dietary supplements, exercise and social support) are not part of the Society for Integrative Oncology’s guidelines because:
- Other groups had already summarized these approaches
- Good evidence was already available about these approaches
The Society for Integrative Oncology advances evidence-based, comprehensive, integrative health care to improve the lives of people with cancer. Members include oncologists, nurses, psychologists, social workers, nutritionists, complementary therapy practitioners, naturopathic doctors, herbalists, acupuncturists and massage therapists.
Guideline Recommendations
Recommendations about each treatment in the guidelines are based on five grades:
- Grade A: Offer the treatment:
High certainty that the treatment has a large benefit - Grade B: Offer the treatment:
High certainty that the treatment has some benefit or
Reasonable certainty that the treatment has some or a large benefit - Grade C: Consider offering the treatment to some patients based on professional judgment and patient preferences:
Reasonable certainty that the treatment has a small benefit - Grade D: Don’t offer the treatment and discourage patients from using it:
Reasonable or high certainty that the treatment has no benefit - Grade H: Don’t offer the treatment:
Reasonable or high certainty that the harms of the treatment outweigh the benefits
The full guidelines are available for free online: “Clinical practice guidelines on the evidence‐based use of integrative therapies during and after breast cancer treatment.”
Leading Cancer Organization Endorses the Guidelines
The American Society of Clinical Oncology (ASCO) endorsed the guidelines in June 2018 as current, accurate and valid. The nearly 45,000 oncology professionals who are members of ASCO are working to conquer cancer through research, education and promotion of the highest quality patient care.
Chart of Complementary and Lifestyle Approaches Supported by Evidence
Evidence shows that these complementary and lifestyle approaches for breast cancer symptoms and treatment side effects are safe and work or may be useful.
ANXIETY AND STRESS
Good evidence that the approach works and is safe
- Exercise and physical activity
- Meditation
- Music therapy
- Social support
- Yoga
Some evidence that the approach may be useful and is safe
- Acupuncture
- Massage therapy
- Relaxation techniques
EATING PROBLEMS
Good evidence that the approach works and is safe
- Healthy eating
Some evidence that the approach may be useful and is safe
- Acupuncture
- Exercise and physical activity
- Ginseng
- Hypnosis
- Social support
- Yoga
(See Healthy Eating under Lifestyle approaches for solutions to specific eating problems.)
FATIGUE
Good evidence that the approach works and is safe
- Exercise and physical activity
Some evidence that the approach may be useful and is safe
- Acupuncture
- Ginseng
- Hypnosis
- Social support
- Yoga
HOT FLASHES
Good evidence that the approach works and is safe
- There are no treatments for hot flashes with good evidence.
Some evidence that the approach may be useful and is safe
- Acupuncture
MOOD PROBLEMS AND DEPRESSION
Good evidence that the approach works and is safe
- Exercise and physical activity
- Massage therapy
- Meditation
- Music therapy
- Relaxation techniques
- Social support
- Yoga
Some evidence that the approach may be useful and is safe
- Acupuncture
- Healing touch
NAUSEA AND VOMITING FROM CHEMOTHERAPY
Good evidence that the approach works and is safe
- Acupressure
- Acupuncture
- Exercise and physical activity
- Healthy eating
Some evidence that the approach may be useful and is safe
- Ginger
- Relaxation techniques
PAIN
Good evidence that the approach works and is safe
- There are no approaches for pain with good evidence.
Some evidence that the approach may be useful and is safe
- Acupuncture
- Healing touch
- Hypnosis
- Music therapy
- Social support
POOR OVERALL QUALITY OF LIFE*
Good evidence that the approach works and is safe
- Healthy eating
- Meditation
- Social support
- Yoga
Some evidence that the approach may be useful and is safe
- Acupuncture
- Qigong
- Reflexology
*Quality of life means your overall ability to function physically, mentally, emotionally and socially.
SLEEP PROBLEMS
Good evidence that the approach works and is safe
- There are no approaches for sleep problems with good evidence.
Some evidence that the approach may be useful and is safe
- Melatonin
- Yoga
LEARN MORE
For more information, see:
- Complementary approaches
- Lifestyle approaches
EASING PAIN THROUGH INTEGRATIVE CARE
Some complementary and lifestyle approaches can help ease pain when they’re combined with conventional treatment. There’s no strong evidence that they work alone though.
Using Complementary and Lifestyle Approaches with Pain Medicines
The most effective treatment(s) begins with determining how bad the pain is. For milder pain, integrative approaches can be part of the pain relief plan, say Dr. Lopez and Dr. Jonas. “Integrative approaches are commonly used together with pain medications to reduce the overall need for pain medications,” says Dr. Lopez.
Doctors start with medications such as acetaminophen (Tylenol) or non-steroidal anti-inflammatory drugs (such as aspirin or Motrin). For severe pain, prescription opioids (narcotics) are an option.
Complementary and lifestyle approaches that can help ease pain when used with medications include:
- Acupuncture
- Healing touch
- Hypnosis
- Music therapy
Social support can help you cope with pain.
“By incorporating several methods for easing pain—conventional approaches coupled with complementary treatments such as acupuncture—we activate our body’s ability to heal,” says Dr. Jonas.
If you have new pain, tell your doctor before trying an integrative approach. “It’s important to know what’s causing the pain before choosing an intervention,” says Dr. Lopez.
Treatments that Don’t Work
The Society of Integrative Oncology has found that these approaches don’t work.
Fatigue:
- Acetyl-L-carnitine
- Guarana
Hot flashes:
- Soy
Nausea and vomiting from chemo:
- Glutamine
COMPLEMENTARY APPROACHES
Complementary approaches are health care approaches that have been developed outside of conventional medicine that are used together with conventional medicine. In cancer care, complementary approaches are used to relieve symptoms of the disease and side effects of treatment.
Mind and body practices are commonly used in cancer care. Mind and body practices combine mental focus, controlled breathing and body movements to help relax the body and mind.
Complementary Approaches
These complementary treatments are safe and work or may be useful for specific breast cancer symptoms and treatment side effects, according to the Society of Integrative Oncology.
Complementary Approaches that Work and are Safe
Acupressure:
- Nausea and vomiting from chemo
Acupuncture:
- Nausea and vomiting from chemo
Massage therapy:
- Mood problems and depression
Meditation:
- Anxiety and stress
- Mood problems and depression
- Poor quality of life
Music therapy:
- Anxiety and stress
- Mood problems and depression
Relaxation techniques:
- Mood problems and depression
Yoga:
- Anxiety and stress
- Mood problems and depression
- Poor quality of life
Each of these approaches is described below.
Complementary Approaches that May be Useful and are Safe
Acupuncture:
- Anxiety and stress
- Fatigue
- Hot flashes
- Mood problems and depression
- Pain
- Poor quality of life
Healing touch:
- Mood problems and depression
- Pain
Hypnosis:
- Fatigue
- Pain
Music therapy:
- Pain
Qigong:
- Poor quality of life
Reflexology:
- Poor quality of life
Yoga:
- Fatigue
Healing touch, hypnosis, qigong and reflexology are briefly summarized after the descriptions of the more common complementary approaches.
Yoga and Acupuncture Help Jessica Filloon Conquer Anxiety and Feel Better
 When Jessica Filloon was diagnosed with breast cancer at the age of 32, she and her husband, John, had a one-year-old son, Harlon, and another child on his way soon. Filloon wanted to do everything she could—along with her conventional cancer care—to heal so she could be there for her family.
When Jessica Filloon was diagnosed with breast cancer at the age of 32, she and her husband, John, had a one-year-old son, Harlon, and another child on his way soon. Filloon wanted to do everything she could—along with her conventional cancer care—to heal so she could be there for her family.
What helped Filloon the most with the anxiety of having cancer, and symptoms of her treatment like fatigue and pain, were yoga and acupuncture.
A Feeling of Helplessness
In August 2016, Filloon was diagnosed with stage III triple negative breast cancer. The Placentia, Calif., resident was 32 weeks pregnant.
“I was supposed to be creating a safe space for the baby inside of me. Instead, I was panicking, thinking I was going to die and wondering what my babies would do without me,” she says.
A team of doctors, including a high-risk OB/GYN, a surgeon and an oncologist at the Kaiser Permanente Orange County-Anaheim Medical Center monitored Filloon’s pregnancy and her cancer. They considered starting chemo right away and having Filloon go full term, but decided it was better to induce labor at 35 weeks and start chemo after delivery. At 35 weeks, they induced labor and performed a C-section.
Two weeks after Wyatt’s birth, Filloon began chemo. Over the next year or so, Filloon had a double mastectomy with lymph node removal, radiation therapy and more chemo. She also had a hysterectomy, because she is BRCA positive, which puts her at increased risk for developing ovarian cancer, as well as a breast cancer recurrence.
“I had my mastectomy when Wyatt was 7 months old. I couldn’t pick him up,” says Filloon. Not being able to care for Wyatt and Harlon was really hard for her.
Yoga Provides Peace of Mind, Helps with Fatigue and Movement
Since she was a teenager, Filloon has practiced yoga on and off. After her diagnosis, she began taking restorative and healing yoga classes at a local yoga studio.
Yoga helped Filloon let go of her fear, get through fatigue from chemo and improve her range of motion after surgery.
Restorative yoga focuses on holding poses for five minutes or more, supported by props that let you relax and rest. During the classes, Filloon was able to let go of anxiety so bad she could barely breathe, and focus on healing and self-care.
“I turned my thoughts into mantras for myself for self-healing, and focused on positive things. I let go of the fear that tried to get into my head,” she says.
During chemo, yoga helped reduce Filloon’s fatigue. After surgery, yoga helped her restore her range of motion. “I wasn’t sure if I’d ever be able to lift my right arm over my head again, but I can. With lots of patience, things have really improved,” she says.
Acupuncture Lessens Pain
Filloon had tried acupuncture before, for pain from migraines and endometriosis. It helped then, so she decided to try it again. This time the target was cancer pain, especially from chemo side effects:
- Bone pain from shots to reduce the risk of infection during chemo
- Never-ending burning pain and peeling skin on her hands and feet
- Sores under her tongue and in other places
- Acupuncture helped ease Filloon’s pain, and also lessened her anxiety.
Back to Family Life
Filloon’s life is very different than it was before. But she is enjoying her “new normal,” and is grateful for her time with her family. She enjoys going for walking adventures and to the beach with three-year-old Harlon, two-year-old Wyatt, and John. She is the team parent for Harlon’s soccer team.
After completing her breast cancer treatment, Filloon took a yoga teacher training program. She now teaches restorative yoga classes at two local yoga studios, and a monthly yoga class for kids. Harlon and Wyatt practice yoga with Filloon at home.
“Going through the training helped me heal even more,” she says. “Now, I’m sharing the healing aspect of yoga, which inspired me, with other people.” Filloon works part-time for a company that provides affordable housing.
ACUPRESSURE
What is Acupressure?
Acupressure stimulates energy flow throughout your body. It is part of traditional Chinese medicine, which believes that energy (qi) flows through pathways (meridians) in the body. To re-balance energy, hands and fingers or a special device are used on specific points along these pathways.
A therapist can do acupressure or you or a family member or friend can do it.
How Do People with Cancer Use Acupressure?
According to the Society for Integrative Oncology, people with cancer use acupressure for:
- Fatigue
- Nausea and vomiting from chemo
- Pain
- Stress
What Does the Evidence Say About Acupressure?
There is good evidence that acupressure relieves nausea and vomiting from chemo when used along with drugs to prevent vomiting, says the Society for Integrative Oncology.
Recommended for:
- Nausea and vomiting during chemo when used along with drugs to prevent vomiting
ACUPUNCTURE
What is Acupuncture?
Acupuncture involves inserting very thin needles through the skin into specific points on your body. This helps you heal by stimulating energy flow throughout your body.
Like acupressure, acupuncture is part of traditional Chinese medicine, which believes that energy (qi) flows through pathways (meridians) in the body. To re-balance energy, acupuncture needles are inserted into specific points along these pathways.
Usually, acupuncture is done with needles. But it can also be done with mild electrical stimulation. This is sometimes called acustimulation or electro-acupuncture.
Acupuncturists, doctors and other health care providers do acupuncture.
In most U.S. states, acupuncturists must be certified by the National Certification Commission for Acupuncture and Oriental Medicine. Some states don’t require certification, but limit which providers can do acupuncture.
How Do People with Cancer Use Acupuncture?
According to the Society for Integrative Oncology, people with cancer use acupuncture for:
- Anxiety and stress
- Hot flashes
- Fatigue
- Nausea and vomiting from chemo
- Pain
- Sleep problems
What Does the Evidence Say About Acupuncture?
There is good evidence that acupuncture relieves nausea and vomiting from chemo, says the Society for Integrative Oncology. Acupuncture may help with some other symptoms and treatment side effects.
Recommended for:
- Nausea and vomiting from chemo
May Help with:
- Anxiety and stress
- Depression and mood problems
- Fatigue after chemo
- Hot flashes
- Pain
- Poor quality of life
Electro-acupuncture could be used during chemo along with drugs to prevent vomiting (antiemetics).
Acupuncture Eases Joint Pain from Aromatase Inhibitors
Acupuncture can reduce joint pain in women with early-stage breast cancer who are taking aromatase inhibitors, says a study published in the Journal of the American Medical Association.
Women with hormone-receptor-positive breast cancer usually take hormonal therapy after surgery to reduce the risk of the cancer coming back (recurrence). Aromatase inhibitors are one type of hormone therapy. They lower estrogen levels in postmenopausal women.
But aromatase inhibitors can also cause muscle and joint pain. The pain can be so bad that women stop taking the medicine.
Researchers at 11 U.S. cancer centers studied 226 women with early-stage breast cancer taking aromatase inhibitors and experiencing joint pain. They divided the women into three groups:
- Acupuncture
- Sham acupuncture
- Waitlist control
After 6 weeks, women who had acupuncture had less joint pain than women who either had sham acupuncture or were in the waitlist control group.
Sham acupuncture is where acupuncture is done, but the needles don’t go as deep and aren’t used in the same places on the body. Participants in the waitlist control group were put on a waiting list to receive acupuncture after the study treatment period ended.
(Source: “Effect of Acupuncture vs Sham Acupuncture or Waitlist Control on Joint Pain Related to Aromatase Inhibitors Among Women With Early-Stage Breast Cancer: A Randomized Clinical Trial,” published in the Journal of the American Medical Association, July 2018.)
MASSAGE THERAPY
What is Massage Therapy?
Massage therapy is rubbing or pressing the soft tissues of your body—muscle, connective tissue, tendons, ligaments and skin—to enhance health and wellbeing.
There are many types of massage, including Swedish, shiatsu and deep-tissue massage. Massage therapists usually use their hands and fingers to do massage, but they may also use their forearms, elbows or feet.
Massage therapy is done by trained and certified medical professionals. For people with cancer, massage therapists should avoid massaging:
- Open wounds, bruises or areas with skin breakdown
- Directly over the tumor site
- Areas with a blood clot in a vein
- Areas that are sensitive after radiation therapy
How Do People with Cancer Use Massage Therapy?
According to the Society for Integrative Oncology, people with cancer use massage therapy for:
- Anxiety and stress
- Pain
What Does the Evidence Say About Massage Therapy?
There is good evidence that massage therapy helps with mood problems and depression, says the Society for Integrative Oncology. It may help with anxiety.
Recommended for:
- Mood problems and depression
May Help with:
- Anxiety
MEDITATION
What is Meditation?
Meditation is a practice to free your mind from stress by focusing on what’s going on in the present moment without any judgment. Doing this for even a few minutes can help you feel calmer and more relaxed.
During meditation you let go of distracting or disturbing thoughts that contribute to anxiety and stress. When your mind wanders back to those thoughts, as it often will, you accept this. Then you re-focus on your breath and body and what’s happening now. It takes time and practice to get comfortable meditating.
Where, How and When to Meditate
You can meditate anytime and anywhere, on your own or in a group class led by instructors trained in meditation. When you’re starting out, it may be easier to learn how to meditate with a teacher. If you mediate on your own, there are many guided meditations online, including through apps. You can also buy DVDs and CDs on meditation. Guided meditations start at 1 minute and many are less than 15 minutes.
Free Guided Imagery to Enhance Your Healing Response
Visit the Dr. Wayne Jonas guided imagery page to access free Health Journeys audios, including:
- A Meditation to Help You Fight Cancer
- Meditations to Release Stress
- A Meditation to Help Ease Pain
Click here to listen to the audios.
Meditation is easier and works best when you do it regularly. Try to find a time that works best for you and make meditation part of your daily routine. Some experts recommend meditating first thing in the morning, to start your day right. You can also meditate whenever you feel stress.
Meditation Basics
Most types of meditation call for:
- A quiet place to meditate, with few distractions
- A comfortable position:
Sitting or lying down - Focused attention:
On breathing, an object, an image or a word or set of words you repeat to help you focus (called a mantra) - An open attitude of letting thoughts come and go in your mind without judging them
Types of Meditation
You’ll probably need to try different types of meditation to see what works best for you and fits your lifestyle.
Mindfulness-based stress reduction is a popular type of meditation that helps you access and build your natural capacity to actively engage in caring for yourself and find greater balance, ease and peace of mind. Usually delivered as an eight-week group course, mindfulness-based stress reduction includes a range of meditation practices, including a body scan, sitting meditation, walking meditation, loving-kindness practice and gentle hatha yoga postures.
Participants practice mindfulness-based stress reduction at home every day.
How Do People with Cancer Use Meditation?
According to the Society for Integrative Oncology, people with cancer use meditation to improve their:
- General wellbeing (quality of life)
- Calmness
- Clarity
- Concentration
What Does the Evidence Say About Meditation?
There is very strong evidence that meditation helps reduce anxiety and stress, improve quality of life and improve mood problems and depression, says the Society for Integrative Oncology. Mindfulness-based stress reduction is very effective for mood problems and depression, based on studies of its use in cancer care, including for breast cancer.
Recommended for:
- Anxiety and stress
- Poor quality of life
- Mood problems and depression
Meditation Relieves Anxiety for New Mom
 Like many breast cancer survivors, Jenny Leyh was really worried that her cancer might come back. Leyh was in the third trimester of her first pregnancy when she was diagnosed with breast cancer. She made it through a year of grueling treatment, focused on delivering a healthy baby and living to take care of her. Leyh’s daughter, Chloë, was
Like many breast cancer survivors, Jenny Leyh was really worried that her cancer might come back. Leyh was in the third trimester of her first pregnancy when she was diagnosed with breast cancer. She made it through a year of grueling treatment, focused on delivering a healthy baby and living to take care of her. Leyh’s daughter, Chloë, was
safely born in June 2016.
But when doctors told Leyh she was cancer free in April 2017, she found herself struggling to push past the physical and emotional trauma of having breast cancer. “Anxiety is the side effect that lingers well beyond the active fight. The fear of a recurrence was debilitating,” she says.
Meditation Makes Scary Thoughts Bearable
Leyh tried many things to feel better, including a low-dose antidepressant and therapy. What worked best for her was something she had never tried before: meditation.
First through YouTube and podcasts, Leyh found that the techniques applied to most exercises—closing the eyes, slowing down the breath and taking three to four deep breaths—were so simple that they could be practiced anywhere. She found herself engaging in some form of meditation every day.
At the very core of mindfulness meditation is the practice of paying attention to the present moment in a non-judgmental way. “I had been through a very difficult experience, and it was difficult to come face-to-face with some thoughts that scared me,” says Leyh. “Through meditation I was able to acknowledge those thoughts without allowing them to consume me.”
Leyh also finds that the mindfulness part of meditation helps her deal with the stress of everyday life. “By training my mind to slow down and focusing on my breathing, the power that stress has over me has been greatly diminished,” she says.
MUSIC THERAPY
What is Music Therapy?
Music therapy is the use of music to treat cancer or other conditions, reduce symptoms or prevent disease or injury. It can include creating, singing, moving to and/or listening to music.
Music therapists are trained to design personalized uses of music for each patient. They are certified in music therapy. Some states regulate music therapists.
How Do People with Cancer Use Music Therapy?
According to the Society for Integrative Oncology and Susan B. Komen, people with cancer use music therapy for:
- Anxiety and stress
- Nausea and vomiting from chemo
- Depression
- Pain
- Poor quality of life
Susan B. Komen is a non-profit organization that fights against breast cancer through research, community health, global outreach and public policy.
What Does the Evidence Say About Music Therapy?
There is good evidence that music therapy helps with anxiety, stress, and mood disorders and depression. There is some evidence that it may help with pain and sleep problems.
Recommended for:
- Anxiety and stress
- Mood problems and depression
May Help with:
- Pain
RELAXATION TECHNIQUES
What are Relaxation Techniques?
When your body is relaxed, you breathe more slowly, have lower blood pressure, and feel an increased sense of wellbeing. Relaxation techniques help produce the body’s natural relaxation response and increase pain-killing substances from the brain.
A therapist or trainer can guide you in relaxation techniques or you can do these on your own.
Types of Relaxation Techniques
Relaxation techniques include:
- Deep breathing exercises
- Progressive muscle relaxation
- Guided imagery (focusing the mind on positive images)
- Autogenic training
- Biofeedback
- Self-hypnosis
Descriptions of each relaxation technique
Deep breathing exercises focus on taking slow, deep, even breaths.
Progressive muscle relaxation involves tensing and relaxing muscles throughout the body. This is often combined with guided imagery and deep breathing exercises.
Guided imagery is a kind of meditation that leads a person’s imagination into a particular state by describing a scene or place and invoking imagery from all of the senses.
Autogenic training involves learning to focus on the physical sensations of warmth, heaviness and relaxation in different parts of your body.
Biofeedback uses an electronic device to measure body functions such as breathing and heart rate and gives you feedback so that you can learn to make changes that facilitate relaxation.
Self-hypnosis involves learning how to produce the relaxation response when prompted by a phrase or a non-verbal cue (called a “suggestion”).
How Do People with Cancer Use Relaxation Techniques?
According to the Society for Integrative Oncology and Susan B. Komen, people with cancer use relaxation techniques for:
- Anxiety and stress
- Depression
- Fatigue
What Does the Evidence Say About Relaxation Techniques?
There is good evidence that relaxation techniques help with mood problems and depression, says the
Society for Integrative Oncology. They may help with anxiety and nausea and vomiting from chemo.
Recommended for:
- Mood problems and depression
May Help with:
- Anxiety and stress
- Nausea and vomiting from chemo
YOGA
What is Yoga?
Yoga is an ancient mind and body practice from traditional Indian (Ayurvedic) medicine. It combines strengthening and stretching poses and deep breathing and meditation or relaxation.
There are more than 100 types of yoga. Some are fast paced and intense. Others are gentle and relaxing. In the United States, hatha yoga is the most common type of yoga practiced. Hatha yoga combines a series of poses with breathing.
People with breast cancer should take a yoga class taught by a certified yoga instructor who has experience working with cancer patients.
How Do People with Cancer Use Yoga?
According to the Society for Integrative Oncology, people with cancer use yoga for:
- Anxiety and stress
- Depression
- Fatigue
What Does the Evidence Say About Yoga?
There is good evidence that yoga helps reduce anxiety, and improve mood problems and depression and poor quality of life, says the Society for Integrative Oncology. Yoga may help with fatigue.
Recommended for:
- Anxiety and stress
- Mood problems and depression
- Poor quality of life
May Help with:
- Fatigue
Other Complementary Approaches
Healing touch involves a trained practitioner who passes his/her hands over, or gently touches, a patient’s body to balance or increase energy (also called therapeutic touch). Uses in cancer: Improve quality of life and reduce pain, fatigue and depression
Hypnosis is a trance-like state, which allows a person to be more aware, focused and open to suggestion. Hypnosis lets a person concentrate more clearly and without distraction on feelings, thoughts, images, sensations or behaviors. It can be done by a trained therapist or as self-hypnosis. Uses in cancer: Help relieve anxiety, stress and pain
Qigong is a mind and body practice that comes from traditional Chinese medicine. It uses movement (physical postures), meditation (focused attention) and controlled breathing. Uses in cancer: Reduce anxiety, fatigue and pain; improve sleep quality; support the immune system; and improve physical and emotional balance
Reflexology involves a trained practitioner who puts pressure on the feet, hands, ears and face using specific thumb, finger and hand techniques. This stimulates changes in the body that can create relaxation and stimulate healing. Uses in cancer: Promote relaxation and improve quality of life
LIFESTYLE APPROACHES
Lifestyle approaches are healthy, evidence-based self-care and behavioral approaches to enhance health and healing. They are used together with conventional medicine. In cancer care, lifestyle approaches are used to relieve symptoms of the disease and side effects of treatment.
This guide covers these types of lifestyle approaches:
- Healthy eating
- Dietary supplements
- Exercise and physical activity
- Social support
“Women with breast cancer who eat healthy food, exercise, and engage in stress management tolerate and complete therapy better, recover faster and suffer fewer consequences of treatment long term,” says Dr. Jonas.
Lifestyle Approaches
These lifestyle approaches may help with specific breast cancer symptoms and treatment side effects, according to the American Cancer Society, the American Institute for Cancer Research, the Society for Integrative Oncology, Susan G. Komen and other experts.
Healthy Eating
- Changes in appetite and weight loss
- Constipation
- Diarrhea
- Fatigue
- Nausea with or without vomiting
- Sore mouth or throat
- Unwanted weight gain
Exercise and Physical Activity
- Anxiety and stress
- Depression
- Fatigue
- Nausea
- Stress
- Weight gain
Social Support
- Anxiety and stress
- Fatigue
- Mood and depression
- Pain
HEALTHY EATING
Evidence About Lifestyle Approaches
Evidence about healthy eating, nutrition and diet in this guide comes primarily from:
- The American Cancer Society
- The American Institute for Cancer Research
- The LIVESTRONG Foundation
- Savor Health™
- Laura Pole, RN, MSN, OCNS, head chef and nurse consultant for the Smith Center for Healing and the Arts in Washington, D.C.
- Rebecca Katz, author of The Cancer-Fighting Kitchen, Second Edition: Nourishing, Big-Flavor Recipes for Cancer Treatment and Recovery.
Why is Healthy Eating Important During Cancer Treatment?
Breast cancer treatments like surgery, radiation therapy and chemo put a lot of demands on your body. Treatments and their side effects, and just having cancer, can affect the way you eat and how your body tolerates certain foods and uses nutrients.
Some cancer treatments work better if you’re well nourished and are eating enough calories and protein.
During many breast cancer treatments, you need extra calories and protein to keep your weight up and heal faster.
Each woman with breast cancer has different nutritional needs. This guide provides an overview of healthy eating
during cancer care in general and ways to deal with common eating problems. Your cancer care team can help you customize this for your needs.
Pre-Packaged Meals Provide Fuel for Jessica Filloon During Chemo
For Jessica Filloon, chemo was like her pregnancies, but “without the bonus of a baby at the end.” The mother of two boys, Harlon, age three, and Wyatt, age two, threw up constantly during both her pregnancies and chemo.
Never hungry during chemo, Filloon started to lose weight. She knew that she needed healthy food to keep up with her treatments and care for her children. But she didn’t want to eat or have the energy to make anything. “Chemo was never-ending nausea and fatigue,” says Filloon.
Healthy, pre-packed meals—breakfasts, lunches, and dinners—made it easier for Filloon to fuel her body. A friend of hers had started a company, called On-Season Meals, which sells pre-packaged healthy meals. “He donated meals to me and my family for a year,” says Filloon.
The ready-to-eat meals made it easier for Filloon to fuel her body with healthy food.
What Does the Evidence Say About Healthy Eating During Cancer Treatment?
The American Cancer Society, the American Institute for Cancer Research and other experts agree that healthy eating is an important part of cancer treatment. According to the American Cancer Society, healthy eating can help you:
- Feel better
- Stay stronger and more energetic
- Maintain a healthy weight
- Give your body key calories and nutrients
- Better tolerate side effects from treatment
- Lower your risk of infection
- Heal and recover faster
“There’s strong evidence that healthy eating helps women with breast cancer feel better during and after treatment.” says Dr. Greenlee.
Most communities offer many resources on healthy eating. Dr. Greenlee suggests asking the nutritionist at your cancer center and your doctor to recommend resources for you. “You don’t need to do it all on your own,” she says.
Nourish and Nurture Your Body, Mind and Spirit
 Food can nourish and nurture your mind and spirit along with your body. “Food is loaded with meaning and emotion. Food is family, tradition and comfort,” says Dr. Jonas.
Food can nourish and nurture your mind and spirit along with your body. “Food is loaded with meaning and emotion. Food is family, tradition and comfort,” says Dr. Jonas.
Feeling Connected to Others and to Life
Laura Pole, RN, MSN, OCNS, agrees. “Eating nourishing and nurturing foods helps people feel connected to each other and to a larger whole,” she says. “You are eating more than protein, carbohydrates, fats and phytonutrients—you are eating life.” Pole is an oncology clinical nurse specialist and health supportive chef who is now head chef and nurse consultant for the Smith Center for Healing and the Arts in Washington, D.C.
What is Healthy Eating for People with Cancer?
During cancer treatment, you should eat:
- Lots of vegetables and fruit
- Moderate amounts of whole grains, and plant protein like nuts, beans, lentils, tofu and tempeh
- Moderate portions of fish, poultry, lean meats and non-fat or low-fat dairy foods
(Source: Heal Well: A Cancer Nutrition Guide (PDF) by the American Institute for Cancer Research, the LIVESTRONG Foundation, and Savor Health™)
Mediterranean Diet Helps Extend Life and Reduce Cancer Risk
The Mediterranean diet consists primarily of fish, vegetables, legumes, whole grains, fruits, extra virgin olive oil, moderate amounts of wine and small amounts of red meat. It limits processed foods and refined sugar.
Studies are showing that following the Mediterranean diet may help:
- Increase survivorship
- Reduce breast cancer recurrence
- Prevent cancer
Sources:
- Mediterranean Diet and Invasive Breast Cancer Risk Among Women at High Cardiovascular Risk in the PREDIMED Trial: A Randomized Clinical Trial
- Adherence to Mediterranean Diet and Risk of Cancer: An Updated Systematic Review and Meta-Analysis The Mediterranean Diet Reduces Breast Cancer Recurrence Risk
Cancer-Fighting Whole Foods
Foods that are as close to their natural form as possible, called whole foods, have more cancer-fighting phytochemicals and nutrients than processed foods. Vegetables, fruits, whole grains, nuts and legumes are all whole foods.
The American Cancer Society suggests eating at least 2½ cups of vegetables and fruits a day, including dark-green and deep-yellow vegetables and citrus fruits.
“Eat real food, mostly from plants,” says Pole. “When you eat foods from the animal kingdom, eat healthier sources.” For example:
- Eat chicken instead of red meat, and buy chicken with few additives
- Buy organic or pasteurized eggs (eggs that have been exposed to heat to destroy potential bacteria)
Make Healthy Food Delicious
 Healthy eating can be delicious too. “You don’t have to be a chef to make food taste good,” says Pole. “Usually if you’re using real food, it already tastes pretty good.”
Healthy eating can be delicious too. “You don’t have to be a chef to make food taste good,” says Pole. “Usually if you’re using real food, it already tastes pretty good.”
Pole and Rebecca Katz, author of The Cancer-Fighting Kitchen, Second Edition: Nourishing, Big-Flavor Recipes for Cancer Treatment and Recovery, both help people with cancer make healthy food delicious.
This is the “yum” factor, says Katz. She starts with ingredients rich in the nutrients that you need to thrive during cancer treatment and creates dishes that are yummy as well as nourishing.
Both Katz and Pole use herbs and spices to add flavor to food and help fight cancer. “Nothing packs more power, gram for gram, than herbs and spices,” says Katz.
For flavorful veggies, try adding:
- Garlic, red pepper flakes, and olive oil to spinach
- Sesame, ginger, and garlic to red cabbage and kale
Katz makes it easy for people with cancer to eat healthy—and yummy—food. “You can have all the nutritional facts and all the science in the world but, at the end of the day, you’ve got kids. You’ve got a life. You just have to get food on the table,” says Katz.
Practical for Your Life
There are four steps to making healthy food a delicious part of your lifestyle:
- Planning
- Advance preparation
- Stocking the pantry and refrigerator
- Willingness to try different things
Katz suggests doing your planning, advance preparation and shopping on the weekend.
Planning includes choosing recipes and developing a shopping list. When you come home with lots of vegetables, prep them for the week by chopping them and putting in airtight containers. “If you’ve already prepped, cooking takes 20 minutes,” says Katz.
Soup is an easy way to eat more vegetables. You can make enough for a few meals and freeze it.
“Small changes make a difference,” says Katz. “Give yourself some credit for making those small changes.
When to Buy Organic Vegetables and Fruits
Vegetables and fruits that are grown without pesticides and synthetic fertilizers—organically—are not only “safer” to eat, but they’re often more nutritious than conventionally grown food. But organic food is expensive.
Lack of Evidence for Anti-inflammatory Diet and Ketogenic Diet
There is no clinical trial-level evidence that the anti-inflammatory diet or the ketogenic diet improves survival in people with cancer.
“You don’t have to eat organic 100% of the time. Just make sure that if you can, you are buying organic where it matters most,” says Katz. She and Pole both recommend following the Environmental Working Group’s annual Shopper’s Guide to Pesticides in Produce™:
- Dirty Dozen™ list
- Clean Fifteen™ list
- The Dirty Dozen™ list highlights what you should buy organic: the 12 vegetables and fruits with the highest levels of pesticide residues.
The Clean Fifteen™ list highlights foods with none or minimal amounts of pesticide residues, where you don’t need to spend extra money for organic.
The list changes each year, so stay current. In 2018, for example, the Environmental Working Group found that 97 percent of conventional spinach samples contained pesticide residues.
Other Recommendations for Healthy Eating
The American Cancer Society also recommends:
- Limiting high-fat foods, especially those from animal sources. Choose low- or no-fat dairy products. Bake or broil foods to reduce fat.
- Limiting salt-cured, smoked and pickled foods The American Institute for Cancer
Research recommends:
- Avoiding processed meats
- Limiting read meat (like beef, pork, lamb) to three portions per week (12-18 ounces)
- Not drinking alcohol, because even small amounts of alcohol consumed regularly increases the risk of breast cancer
Get more information and download
EWG’s Healthy Living App.
If you can’t do some or any of these things, your cancer care team can help you find a way to get the nutrition and nourishment you need.
Stocking Your Cancer-Fighting Kitchen
Fill your refrigerator and pantry with ingredients for healthy meals that will help you feel better during cancer treatment and deal with common eating problems.
Herbs and spices, such as:
- Cayenne
- Cardamom
- Cinnamon
- Garlic
- Ginger
- Mint (fresh)
- Parsley (fresh)
- Nutmeg
- Oregano
- Turmeric
Healthy fats:
- Avocado oil
- Extra virgin olive oil
- Ghee
- Sesame oil
Acids:
- Lemon juice (fresh)
- Lime juice (fresh)
- High-quality vinegar
Fresh vegetables and fruits, especially those that are deep in color:
- Apples
- Blueberries
- Carrots
- Dark leafy greens
- Onions
- Sweet potatoes
- Tomatoes
- Winter squash
Other:
- Sea salt
- Dark amber organic maple syrup
- Beans
- Whole grains such as quinoa and brown rice
- Lentils
- Nuts
What Can Help with Common Eating Problems?
Common eating problems from breast cancer treatment are:
- Changes in appetite and weight loss
- Constipation
- Diarrhea
- Fatigue
- Nausea with or without vomiting
- Sore mouth or throat
- Unwanted weight gain
The evidence covered for what can help you cope with these problems comes from:
- Heal Well: A Cancer Nutrition Guide (PDF) (by the American Institute for Cancer Research, the LIVESTRONG Foundation, and Savor Health™)
- American Cancer Society, How to cope with common eating problems
Ready-to-Eat High-Calorie, High-Protein Foods
• Avocado
• Canned tuna or chicken
• Cheese
• Dried fruits
• Guacamole
• Hard-boiled eggs
• Hummus on whole grain crackers or bread
• Liquid nutritional supplements
• Ice cream (low sugar)
• Nuts
• Peanut butter and almond butter (natural with no sugar added)
• Pudding (low sugar)
• Yogurt
Changes in Appetite and Weight Loss
- Eat more often: five or six small meals or meals and snacks.
- Drink most of your liquids between meals (unless your mouth is dry and you need liquids more often).
- Eat high-protein foods first.
- Keep high-calorie, high-protein snacks handy.
- Be as physically active as you can so you’ll feel hungrier.
- Ask friends and family to help you buy and prepare foods.
Constipation
- Drink more healthy drinks, especially water, prune juice, warm juices, decaffeinated teas and hot lemonade.
- Eat more high-fiber foods, like whole-grain bread and cereals, raw and cooked vegetables, fruit, nuts, seeds and dried beans. Check with your cancer care team to make sure this is okay for you. Your team may also recommend a high-calorie, high-protein liquid supplement with fiber.
- Be as physically active as you can.
- Work with your cancer care team to set up a plan. This may include stool softeners and gentle laxatives.
- Use laxatives only as directed by your cancer care team. Contact your team if you haven’t had a bowel movement for three days or longer.
Diarrhea
- Drink plenty of liquids, like water, clear juices, sports drinks, broth or weak tea. Drink liquids at room temperature. After each loose bowel movement, drink at least 1 cup of liquid.
- Eat small, frequent meals and snacks of soft, bland foods, like bananas, white rice, applesauce and white toast.
- Eat more fiber, like whole-grain bread and cereals, raw and cooked vegetables, fruit, nuts, seeds and dried beans.
- Avoid foods that are greasy, fried, spicy or very sweet.
- Drink or eat no more than 2 cups a day of milk or milk products, including yogurt and buttermilk.
- Take anti-diarrhea medicine if your cancer care team prescribes this.
Preventing Diarrhea from Chemo
Lactobacillus is one of the main types of friendly bacteria in probiotics. It may help prevent diarrhea due to the chemo drug 5-fluorouracil, says the Natural Medicines database. Lactobacillus is in some fermented foods like yogurt, kefir and kimchi and in dietary supplements.
Fatigue
- Eat low effort, ready-to-eat foods like hard boiled eggs, nut butters, fruits and vegetables until you feel stronger; avoid high carbohydrate food with refined sugars like candy, cupcakes, muffins, chips and crackers until you feel stronger.
- Make extra food when you feel stronger and freeze meal-size portions.
- Drink plenty of fluids, because dehydration can make fatigue worse. Drink at least eight cups of fluid daily, like water, clear juices, sports drinks, broth or weak tea. If you’re losing weight, drink some fluids that have calories, like juices or milk.
- Eat some protein, fat and fiber with each meal and snack.
- Ask friends and family to help you buy and prepare foods.
- Ask for a referral to a dietitian.
Eating During Chemo
Eat a light meal or snack about an hour or so before chemo, says the American Cancer Society. If you’ll be there a few hours, bring a small meal or snack. Use an insulated bag or cooler or ask if there’s a refrigerator or microwave you can use. Some oncologists say that fasting 24 hours before chemo can reduce side effects. But this hasn’t been tested in quality research. Don’t do this if you’re underweight.
Nausea with or without Vomiting
- Eat small meals and snacks 6 to 8 times a day.
- When you wake up and every few hours, eat dry foods, like crackers, toast, dry cereals or bread sticks.
- Eat foods and drink liquids at room temperature.
- Avoid foods with strong odors.
- Avoid hot, spicy, greasy, fried, high-fat or very sweet foods.
- If you need to rest, sit up or recline with your head raised for at least an hour after eating.
- Sip clear liquids, like broth, sport drinks, water, and juice often between meals to prevent dehydration. If you’re vomiting, drink clear liquids as often as possible, starting about 60 minutes after you have vomited. Drink sips of a clear liquid or take bites of ice.
- On treatment days, eat bland, soft, easy-to-digest foods like Cream of Wheat and chicken noodle soup with saltines.
- Avoid eating in a room that’s warm, or that has cooking odors or other smells. Cook outside on the grill or use boiling bags to reduce cooking odors.
- Suck on hard candy, like peppermint or lemon, if there’s a bad taste in your mouth.
- Ask your doctor about medicines to prevent or stop nausea.
Preventing Nausea and Vomiting During Chemo
Ginger may help with nausea and vomiting from chemo, along with drugs that prevent or treat nausea and vomiting, says the Society for Integrative Oncology. There is a reasonable certainty that ginger has a small benefit. Ginger is available in capsules, fresh as a root, in tea or in candy. But according to LIVESTRONG, too much ginger can act like a blood thinner, causing excessive bleeding if you’re taking medicines like aspirin or ibuprofen.
Sore Mouth or Throat
- Eat soft, moist foods like cream soups, cheeses, mashed potatoes, yogurt, eggs, custards, puddings, cooked cereals and canned liquid food supplements.
- Avoid foods that are:
- Dry, coarse, or rough, like crackers, nuts, granola, and raw fruits and vegetables
- Tart, acidic or salty
- Pickled or vinegary
- Tomato-based
- Avoid caffeine and alcohol
- Choose soothing lukewarm or cold foods, like frozen fruits, frozen fruit pops or ices, or ice chips.
- Blend or liquefy foods to make them easier to swallow.
- Drink warm or cool liquids, like milk, non-acidic fruit drinks (which you can dilute) and soup.
- Ask your doctor about medicines to numb or soothe your mouth or throat.
- Have your doctor check to be sure you don’t have thrush, which is an oral yeast infection.
Coping with Unwanted Weight Gain
More than half of women with breast cancer experience weight gain during treatment, says Cancer.Net, information for patients from the American Society of Clinical Oncology.
Treatments like chemo, steroids and hormone therapy can all make you pack on the pounds. Doctors may tell you not to worry about this while your body is fighting cancer. But if you want to try to control your weight, healthy eating and physical activity can help.
Here are a few things to try:
- Feel fuller by eating mostly foods that are low in calories and high in fiber, like vegetables, fruits, whole grains and beans. But also treat yourself to a little bit of the higher calorie foods you really like.
- Limit fat, sugar and refined flour.
- Drink plenty of water.
- Use healthier ways to cook, like steaming instead of frying.
- Find physical activities that you like, like walking or bicycling.
- Try strength-building exercises if you’ve lost muscle.
But check with your doctor before starting to exercise or increasing what you’re doing.
DIETARY SUPPLEMENTS
What are Dietary Supplements?
Dietary supplements include vitamins, minerals, herbs or products made from plants, animal parts, algae, seafood or yeasts. They come in many forms, including tablets, capsules, liquids, teas, concentrates and powders.
The quality of dietary supplements varies. Some are made in clean, controlled laboratories and have accurate labels. Others are not and may not have any of the substances listed on their labels. Some dietary supplements contain other substances that are not on their labels and are harmful.
Dietary supplements may have risks and side effects. In the United States, sellers don’t have to show that the supplements are safe and effective. A lot of the information about dietary supplements is wrong. Always talk to your doctor before using any dietary supplement. If you’re already taking dietary supplements, let your doctor know about them.
How Do People with Cancer Use Dietary Supplements?
According to Heal Well: A Cancer Nutrition Guide (PDF) (by the American Institute for Cancer Research, the LIVESTRONG Foundation, and Savor Health™), people with cancer use dietary supplements:
- To strengthen their immune systems
- To help with symptoms and side effects of cancer and cancer treatment
- Because they hope dietary supplements will stop the cancer
Eat Whole Foods Instead
Whole foods, like vegetables, fruits, whole grains, nuts and legumes, are packed with cancer-fighting phytochemicals and nutrients. Eat these instead of relying on dietary supplements.
What Does the Evidence Say About Dietary Supplements?
The use of dietary supplements during cancer treatment is controversial. Doing this can be dangerous.
Dietary supplements may interact with your cancer treatment and make the treatment less effective, according to Heal Well: A Cancer Nutrition Guide (PDF). Some studies show that large doses of dietary supplements prevent destruction of cancer cells. Other studies don’t show this.
Danger: Don’t Take St. John’s Wort or Acetyl-L-carnitine
St John’s Wort can help relieve depression and fatigue, but it also may:
- Make chemotherapy less effective
- Increase skin problems from radiation therapy
Acetyl-L-carnitine (ALC), long thought to help nerve damage from chemo, makes this worse.
Many cancer experts advise their patients not to take dietary supplements during cancer treatment. Sometimes they suggest a specific dietary supplement to treat a cancer symptom or a treatment side effect.
Only use dietary supplements in collaboration with your cancer care team. If you’re already taking dietary supplements, talk to your doctor about them.
The Danger of Dietary Supplements
Up to 80 percent of people with cancer have taken dietary supplements before being diagnosed with cancer, during treatment or afterwards, says the American Institute for Cancer Research. Many people think that dietary supplements are safe, because they’re natural and you don’t need a prescription to buy them.
“Just because something is natural doesn’t mean it’s safe or effective or harmless,” says Dr. Greenlee.
“Natural products have known side effects.”
Less Effective Treatment and More Side Effects
“We’re concerned about interactions between some dietary supplements and chemo, radiation and healing from surgery,” says Dr. Greenlee. For example:
- Some dietary supplements can make the skin sensitive, which causes severe skin reactions during radiation therapy
- Some herbs can make chemo drugs less effective or cause side effects such as bleeding
- Antioxidants may stop conventional cancer treatments from killing cancer cells
Along with interfering with cancer treatment, there’s little evidence to support the use of dietary supplements. “Very few dietary supplements have been shown to be useful to prevent or treat breast cancer symptoms and side effects,” says Dr. Greenlee.
Self-Healing through Naturopathic Medicine
Women with breast cancer who come to the Seattle Cancer Care Alliance’s Integrative Medicine Program are often already taking dietary supplements. “We help our patients understand where we do and don’t have evidence for the use of dietary supplements,” says Dr. Greenlee.
As a naturopathic doctor, Dr. Greenlee has extensive training in nutrition and dietary supplements. She evaluates each patient and makes recommendations about the best types of supportive care during cancer treatment.
Naturopathic medicine uses natural therapies to treat the whole person and encourage the self-healing process. It uses a broad approach to integrative breast cancer care, including:
- Acupuncture
- Healthy eating
- Exercise
- Stress reduction
Rigorous Training for Naturopathic Doctors
Dr. Greenlee and other naturopathic doctors complete a four-year clinical program. The first two years are similar to conventional medical school. During the last two years, students have hands-on training in outpatient programs.
Along with the standard medical subjects, students learn about subjects such as clinical nutrition, acupuncture, botanical medicine, physical medicine and counseling. Most students do not do training beyond that, like in a residency or fellowship alongside conventional doctors.
Naturopathic physicians work in private practices, hospitals, clinics and community health centers. Currently 20 states, including Oregon, and the District of Columbia, Puerto Rico, and the U.S. Virgin Islands, license or certify naturopathic doctors.
Learn more about naturopathic medicine from the American Association of Naturopathic Physicians.
4 Safe Dietary Supplements
There is enough evidence about the safety of a few dietary supplements to consider their use for specific cancer symptoms and treatment side effects:
- Ginger to relieve nausea and vomiting from chemo
- Ginseng to reduce fatigue
- Lactobacillus to prevent diarrhea
- Melatonin for sleep problems
You should still talk to your doctor before using any of these dietary supplements.
Four Safe Dietary Supplements
Ginger is an herb that may help with nausea and vomiting from chemotherapy, along with drugs that prevent or treat nausea and vomiting, says the Society for Integrative Oncology. There is a reasonable certainty that ginger has a small benefit. Ginger is available in capsules, fresh as a root, in tea, or in candy.
But according to LIVESTRONG, too much ginger can act like a blood thinner, causing excessive bleeding, if you’re taking medicines like aspirin or ibuprofen.
Ginseng is an herb that may help reduce fatigue during cancer treatment when the ground root is used, says the Society for Integrative Oncology. There is a reasonable certainty that ginseng has a small benefit. But according to the Natural Medicines database, ginseng could cause a fast heartbeat called tachycardia and increase the risk of bleeding.
Lactobacillus is one of the main types of friendly bacteria in probiotics. It may be effective for preventing diarrhea due to the chemo drug 5-fluorouracil, says the Natural Medicines Comprehensive Database. Lactobacillus is in some fermented foods like yogurt and in dietary supplements.
Melatonin is a hormone in the body that’s also made into a medicine in a laboratory, most commonly as pills. It’s likely effective for trouble falling asleep and possibly effective for insomnia, says the Natural Medicines database.
EXERCISE AND PHYSICAL ACTIVITY
Evidence About Exercise and Physical Activity
Evidence about exercise and physical activity in this guide comes from:
- The American Cancer Society
- The American Institute for Cancer Research
- The LIVESTRONG FoundationSavor Health™
Why are Exercise and Physical Activity Important During Cancer Treatment?
Breast cancer treatments like surgery, radiation therapy and chemo put a lot of demands on your body. Treatments and their side effects, and just having cancer, make you feel bad physically and emotionally.
Moderate exercise during cancer treatment can give you more energy, improve your mood and help relieve some of the symptoms of cancer and side effects of treatment.
Each woman with breast cancer has different needs. This guide provides an overview of exercise during cancer treatment in general. Your doctor or cancer care team can help you develop an exercise program that is right for you.
“There’s a lot of strong evidence that physical activity helps women with breast cancer feel better during and after treatment.” says Dr. Greenlee.
Talk to Your Doctor Before Exercising
Whether you exercised before you were diagnosed with breast cancer or are new to exercise, talk to your doctor before exercising during cancer treatment.
Know When Not to Exercise
There are times you shouldn’t exercise during cancer treatment. These times include if you have:
- A low red blood cell count (anemia)
- Abnormal levels of sodium, potassium and other minerals in your blood from vomiting or diarrhea
- Unrelieved pain, nausea with or without vomiting or any other symptom that concerns you.
Know What’s Safe for You
Your doctor can also tell you what is and isn’t safe for you. For example, if you’re:
- Getting radiation therapy, don’t expose your skin to chlorine in swimming pools.
- Getting chemo or radiation therapy, stay out of the sun.
- Less able to fight infection because of low white blood cell counts or medicines you take, don’t exercise in public places.
- Older, or have cancer that’s spread to the bones or medical problems like osteoporosis or arthritis, you may need someone to help you when you exercise.
What Does the Evidence Say About Exercise and Physical Activity?
Research shows that regular moderate exercise can improve how well you function and your quality of life during and after cancer treatment. Research also shows that exercise is safe for people with cancer.
The American Institute for Cancer Research says that exercise:
- May help you tolerate cancer treatment better
- Can improve endurance, wellbeing and self-esteemBoth the American Institute for Cancer Research and the American Cancer Society say that exercise can lessen symptoms of cancer and side effects of treatment, like:
- Anxiety
- Depression
- Fatigue
- Nausea
- Weight gain
Stress can also be relieved with exercise, says the American Institute for Cancer Research.
Other general benefits of exercise include:
- Improving balance and lowering the risk of falls and broken bones
- Keeping muscles from getting weak
- Lowering the risk of heart disease, osteoporosis and blood clots
- Helping you be more independent with your everyday activities
Customized Exercise Plans at MD Anderson
Exercise during breast cancer treatment is one of the best ways to ease many symptoms and side effects, says Dr. Lopez. At MD Anderson, an integrative medicine physical therapist develops customized exercise plans for each patient, focusing first on safety.
After reviewing the patient’s medical history, cancer treatment, fitness level and health goals, the physical therapist and the patient work together to develop the plan. The exercise plan can be for exercising at or outside the home, based on the patient’s preference.
The physical therapist shows the patient how to do the exercises. The physical therapist or another member of the integrative medicine team will monitor the exercise plan.
Exercise Consultations for Active Women
MD Anderson recommends an exercise consultation even for women who were very active before starting treatment for breast cancer. Changes to an exercise program are probably needed, since treatment causes fatigue and can affect how the body responds to exercise.
What Type of Exercise and Physical Activity is Recommended?
Your exercise program should help you stay as active and fit as possible during cancer treatment. It should be based on:
- What’s safe for you
- Any exercise you’re already doing
- What will work best for you
- What you like doing
The American Cancer Society recommends regular exercise:
- At least 150 minutes a week, if you can
- Moderate exercise along with at least 2 days a week of strength training exercises (e.g., lifting weights)
How to Exercise
Moderate exercise, which works your heart, has the most health benefits. Examples of moderate exercise are:
- A brisk walk
- Water aerobics
- Riding a stationary bike
- Light yoga
- Tai chi or qigong
Your doctor will probably recommend that you exercise and offer some suggestions. Many cancer centers have exercise classes designed for the needs of people with cancer.
If these classes aren’t convenient for you, or your cancer center doesn’t offer them, check out LIVESTRONG at the YMCA. In this free or low-cost exercise program for people with cancer, a certified fitness instructor will develop a customized exercise program for you. The instructors are trained in cancer survivorship, post-rehabilitation exercise and supportive cancer care.
Tips on Exercise and Physical Activity
Starting an Exercise Program
- Do what you can. Listen to your body when you exercise. Don’t push yourself while you’re having treatment.
- Start slowly. Even a few minutes a day of exercise will help you. Try to exercise for at least 10 minutes at a time. Increase how much time you exercise slowly over a few weeks. Try to build up to 30 minutes a day.
- Exercise in short sessions. Ten minutes of exercise three times a day works as well as 30 minutes of exercise at one time. Rest whenever you need to.
Adding Physical Activity to Your Day
You can also add physical activity to your daily life, when you feel well enough. Here are some ways to do this:
- Take a short walk around your neighborhood
- Play active games with kids, like tag
- Use the stairs instead of the elevator
- Park far away and walk to a building
- Wash your car
- Clean your bathroom
More Tips on Exercise and Physical Activity
Get more tips from the American Cancer Society.
SOCIAL SUPPORT
Social support is now usually considered mainstream cancer care, not integrative medicine. The Society for Integrative Oncology, Dr. Jonas, and other experts say there is a strong evidence base for social support.
We’ve included social support in this guide because it’s part of the optimal healing environment described by Dr. Jonas in How Healing Works. “Social and professional interactions that foster a sense of belonging, wellbeing and coherence are healing relationships. Nurturing healing relationships are one of the most powerful ways to stimulate, support and maintain wellness and recovery,” he says.
Evidence About Social Support
Sources of evidence about social support in this guide include:
- Wayne Jonas, MD, How Healing Works
- Society for Integrative Oncology
- Susan G. Komen
Why is Social Support Important for People with Cancer?
No matter how strong you are emotionally, every woman with breast cancer can use social support.
“A diagnosis of breast cancer and its treatment touches on all aspects of a woman’s identity and functioning,” says Kauser Ahmed, PhD, director of the Simms/Mann UCLA Center for Integrative Oncology at UCLA Jonsson Comprehensive Cancer Center, an NCI-Designated Comprehensive Cancer Center. Dr. Ahmed is also the Darcie Denkert Notkin director of psychosocial oncology care, a staff clinical psychologist, and a licensed psychologist.
Along with the physical impacts of breast cancer treatment, you face changes in your appearance and difficulty doing the things that you used to do. “Having support helps you understand that you’re not alone, that the changes you’re experiencing are normal, and that you are one of many women facing these challenges,” says Dr. Ahmed.
Breast cancer also affects your family members. Social support helps you and your family members feel loved, cared for and understood.
“Seeking support really enhances your sense of feeling validated and empowered. It doesn’t mean you’re weak or a victim,” says Dr. Ahmed.
What is Social Support for People with Cancer?
Social support is emotional support, practical help and advice. Common types of social support are:
- Informal support and help from family and friends
- Support groups
- One-on-one counseling
- Online communities
- Tools to communicate with family and friends like Caring Bridge
“These tools can help you navigate the breast cancer experience, rather than figuring it out on your own,” says Dr. Ahmed.
Practical Help
Social support from family and friends often includes practical help like:Rides to and from treatments
- Help with grocery shopping or cooking
- Help taking care of your kids
- Help cleaning your home
Often, family and friends want to help but don’t know what to do. Let them know what you need and how they can help you.
Dikla Benzeevi Thrives Despite Metastatic Breast Cancer
 In the 16 years since being diagnosed with stage III breast cancer at age 32 and metastatic stage IV breast cancer at age 34, Dikla Benzeevi has been riding a scary roller coaster. Benzeevi’s diagnosis was especially scary because her mom died from breast cancer when she was 14. The uncertainty and ups and downs of life with breast cancer got far worse when Benzeevi’s cancer spread to her bones in 2004 and then to her lungs in 2007.
In the 16 years since being diagnosed with stage III breast cancer at age 32 and metastatic stage IV breast cancer at age 34, Dikla Benzeevi has been riding a scary roller coaster. Benzeevi’s diagnosis was especially scary because her mom died from breast cancer when she was 14. The uncertainty and ups and downs of life with breast cancer got far worse when Benzeevi’s cancer spread to her bones in 2004 and then to her lungs in 2007.
“My world turned upside down, and I was lost,” says Benzeevi, who lives in Los Angeles. As she began her treatment at UCLA Jonsson Comprehensive Cancer Center, one of her doctors told her about the Simms/Mann UCLA Center for Integrative Oncology, and even walked her to the center’s door.
Support Group Provides Comfort and Information
As Benzeevi went through her initial treatment—chemo, radiation therapy, lumpectomy and lymph node dissection—she participated in the weekly Breast Cancer Support Group. “I got to meet women going through what I was going through and got the guidance of expert counselors,” she says. “The group gave me the comfort of knowing I had somewhere to go with any questions I had. I was not alone in this process and did not have to blindly figure my
way around.”
The Search for Younger Women with Breast Cancer
But Benzeevi hadn’t been able to find other young women with breast cancer near her. When she heard about the Young Survival Coalition annual conference, she decided to go. Started by three women who were under the age of 35 when they were diagnosed with breast cancer, the coalition offers resources, connections and outreach, and runs regional and national conferences and local in-person support groups for women who were diagnosed with breast cancer at age 40 or younger.
Then Benzeevi established an informal support network for young women with breast cancer on the West Coast, which grew to more than 1,000 members. Benzeevi ran the group from 2004 to 2010.
Support from Other Women with Metastatic Breast Cancer
In 2004, Benzeevi found out that her breast cancer had spread to her bones, and badly fractured one of the vertebra in her spine. Doctors immediately put her in a chin-to-waist back brace to protect her spine. They told her the tumor growth and spine fracture could lead to spinal cord damage and paralysis. Benzeevi later had spine fusion surgery to prevent this.
Breast cancer that’s spread to another part of the body is stage IV, or metastatic breast cancer. Also called MBC, metastatic breast cancer can’t be cured. But it can be treated.
The weekly Living Beyond Limits support group at the Simms/Mann UCLA Center for Integrative Oncology gives Benzeevi comfort and helps her stay balanced. “I had my family support. I had the members of my young women with breast cancer support group. But this group understands what advanced stage cancer patients go through every day,” she says.
“Most of the time, we look okay on the outside. No one can see we’re dealing with a life-threatening illness. But we have a lot of turbulence in our lives. How much time do we have on this earth? How do we live a life that’s full of uncertainly, risks, side effects and difficult ailments? How can we live a life that’s meaningful, and can still produce joy and fulfillment?”
In 2007, Benzeevi’s breast cancer spread again to her lungs, and she had surgery to remove part of one lung. She’s been in treatment for cancer since her diagnosis in 2002, including 14 chemotherapy and other cancer drugs.
Counseling and Hope to Live in the Best Way Possible
Individual counseling at the Simms/Mann UCLA Center for Integrative Oncology has helped Benzeevi get through the worst times. “I’ve had periods of deep depression. As a human being, there’s only so much hardship and distress I can handle,” she says. Benzeevi sees Kauser Ahmed, PhD, center director. “Kauser helps me build constructive coping habits and get through cancer’s turbulent effects on my life day-by-day in the best way possible,” says Benzeevi.
The Simms/Mann UCLA Center for Integrative Oncology gives Benzeevi hope. “Hope is about living in reality in the best way possible while dealing with cancer. The staff are all about providing hope to us in a kind, compassionate, supportive, comprehensive and expert manner.”
Giving Support as a Patient Navigator and Advocate
Helping other women with breast cancer, as a peer counselor and patient advocate, is Benzeevi’s passion. As a trained peer counselor for breast cancer organizations, she counsels patients, survivors and their families on medical, financial and support services.
“We’re all one big community. There are ways for ourselves, our families and our communities to get through each day and make it the best possible while living with cancer by building strong connections and networks with others and each other,” she says.
Benzeevi advocates to improve the quality and length of life for people with metastatic breast cancer, working with breast cancer organizations, researchers, community groups and policymakers. She regularly speaks about breast cancer issues at local, national and international meetings.
Facebook Community for Metastatic Breast Cancer Thrivers
Benzeevi calls herself a metastatic breast cancer “thriver.” In 2015, she created Thriving with Advanced Metastatic Stage 4 Breast Cancer, which is one of the largest Facebook support groups for people with metastatic breast cancer. The group provides a safe, compassionate place for sharing and discussing metastatic breast cancer experiences and providing and receiving support, hope, encouragement and information.
While social media doesn’t provide the comfort of a live support group, it’s a great way for women throughout the country to meet and support each other. Benzeevi’s Facebook group helps women living with metastatic breast cancer who want to connect with others in a similar situation find emotional support, share experiences, learn about treatments and find the best ways to deal with side effects and any other issues that come up related to their cancer experience.
Seek Support
“Don’t go though this alone,” says Benzeevi. “Find your peer network and your support network and learn about what’s out there for you regarding treatments and improving your quality of life. There’s a huge community out there that supports you.”
Support Groups
Support groups help women with breast cancer share their concerns with each other and learn more about how to cope with breast cancer. They help you understand that you’re not alone in your breast cancer experience.
Some support groups mainly provide information and education. Others focus on emotional support. They usually meet once a month or once a week.
Support Groups at Simms/Mann UCLA Center for Integrative Oncology
Being strong, positive and brave when you have breast cancer isn’t easy. Yet many women try to do this for their families, despite the many physical, cognitive and emotional impacts of breast cancer.
Support groups provide a safe and supportive space where women can be honest about what they’re going through and know that they’re not alone. “Support groups create a sense of community with other women who are experiencing a similar diagnosis and treatment,” says Valentina Ogaryan, PhD, clinical psychologist and facilitator of the Breast Cancer Support Group at the Simms/Mann UCLA Center for Integrative Oncology at UCLA Jonsson
Comprehensive Cancer Center, an NCI-Designated Comprehensive Cancer Center.
A Healing Experience
The blend of community, sharing, problem-solving and education in support groups helps women with breast cancer heal. Research shows that support groups can help reduce anxiety and depression while optimizing wellbeing and helping people cope with cancer.
“Breast cancer support groups are not just for people who are struggling or sad,” says Dr. Ahmed. “The whole gamut of emotions that are part of being human are part of the group. There’s a lot of laughter, a lot of poignant emotion, a lot of love, and sometimes sadness and tears.”
A support group isn’t a pity party, adds Dr. Ogaryan. “It’s an additional opportunity to strengthen your existing coping skills,” she says.
A Variety of Support Groups
The Simms/Mann UCLA Center for Integrative Oncology offers a variety of support groups, some of which focus more on talking and others on doing, says Dr. Ahmed. Some groups are for all cancer patients and family members, while others are for patients or family members only.
The weekly Breast Cancer Support Group and Living Beyond Limits are “talking” groups for breast cancer patients. The Breast Cancer Support Group helps women from diagnosis through treatment, while Living Beyond Limits is for patients with cancer that came back or is metastatic.
“Some women are comfortable doing a lot of sharing. Some women come regularly and don’t say much. Both types of women are getting what they need,” says Dr. Ahmed. “You aren’t expected to share every private detail of your life in a support group.”
Healing Through Art is a popular weekly support group that uses drawing, painting, box making, collage, etc., to explore, reveal and express the issues faced by cancer patients.
Skills and Support
Some groups at the Simms/Mann UCLA Center for Integrative Oncology help participants learn skills to cope with cancer while providing support. “These groups combine learning skills and ideal ways to navigate and manage challenges within a sense of community,” says Dr. Ahmed. They include different types of meditation and other mind-body approaches to coping with cancer.
In Mindfulness Meditation, for example, each session begins with a period of sharing, followed by reflection on a specific tool or technique. Participants practice the tool or technique for about 20-30 minutes. The session concludes with more sharing on the experience of using the tool or technique.
Staff members at the Simms/Mann UCLA Center for Integrative Oncology encourage all cancer patients to try a support group, and attend a few times, to see if it’s helpful. “Don’t assume you are not a support group person. When a group is well run, everyone can gain a lot and give a lot,” says Dr. Ogaryan.
Counseling and Other Support Services
Like support groups, counseling also offers a safe, supportive atmosphere for processing feelings and emotions related to having breast cancer. Counseling is helpful in developing specific strategies for coping with breast cancer and for dealing with multiple stresses beyond cancer. It’s available for patients and family members and may include mind/body techniques such as relaxation and guided imagery.
Many women with breast cancer who come to the Simms/Mann UCLA Center for Integrative Oncology have one or two counseling sessions to identify needs and develop a plan. The plan could include joining a support group, taking a workshop such as cognitive behavioral therapy for sleep during cancer, and/or meeting with the center’s integrative nutritionist. Women with more stress in their lives may benefit from ongoing counseling or seeing the
center’s psychiatrist.
The Simms/Mann UCLA Center for Integrative Oncology also offers nutrition, supplements, complementary care and spiritual care.
Counseling
One-on-one counseling, or therapy, gives you a chance to sit down and talk with a counselor about your worries and concerns. The counselor can also help you learn how to cope with the stress of having breast cancer, for example, through training in coping skills or relaxation exercises.
Get Support from Breast Cancer Survivors
Get one-on-one support from someone who understands what you’re going through: a breast cancer survivor.
Volunteers in the American Cancer Society’s Reach to Recovery program will talk with you about how to cope with having breast cancer and getting through treatment. They can support you through face-to-face visits or by phone.
Call 1-800-227-2345 to get matched with a Reach to Recovery volunteer.
Online Communities
Free online communities like the Cancer Survivors Network and Caring Bridge let you:
- Express your feelings and experiences
- Get and provide support
- Keep family and friends updated. The American Cancer Society’s Cancer Survivors Network is a
community of cancer survivors, families and friends that shares personal stories, participates in
discussions, and shows care and support. Features include:
- “CSN My Space,” where you can tell your story, recommend resources and more
- Internal email to other members
- Discussion boards and chat rooms
- Personal support community of CSN members Caring Bridge is a non-profit organization that lets you create a personal website to communicate with family and friends and keep them updated. You can:
- Share news and updates
- Communicate privately
- Coordinate the help you need
- Get support
The American Cancer Society also offers MyLifeLine.org. Like Caring Bridge, this online community lets you set up a personal web page. The Helping Calendar feature lets you organize help with meals, rides to treatment, and more and review and share reliable cancer resources.
The Young Survival Coalition, for women diagnosed with breast cancer at age 40 or younger, offers an online and live community, resources, and outreach to young women with breast cancer. The YSC Discussion Boards, online video support groups, and a Facebook group offer opportunities to connect online. Live activities include regional and national conferences and local in-person support groups.
Jessica Filloon Searches for Women Like Her
 As a young woman with breast cancer and a mom of young children, Jessica Filloon felt like an outcast. “In the chemo chair, I was the youngest person in the room,” she says. While the Kaiser Permanente Orange County-Anaheim Medical Center where she had her treatment offered support services, Filloon knew that she wouldn’t meet other women like her.
As a young woman with breast cancer and a mom of young children, Jessica Filloon felt like an outcast. “In the chemo chair, I was the youngest person in the room,” she says. While the Kaiser Permanente Orange County-Anaheim Medical Center where she had her treatment offered support services, Filloon knew that she wouldn’t meet other women like her.
Connecting with Other Young Moms with Breast Cancer
“I wanted to find my own group of people,” says Filloon, who did this through Facebook, Instagram, and the Young Survival Coalition.
By posting on mommy blogs on Facebook, Filloon found a group of women who were diagnosed with breast cancer while they were pregnant or shortly after they had their babies. Some of the women lived close enough for Filloon to meet with them in person. Through the San Diego group of the Young Survival Coalition, Filloon met other women like her.
Filloon got and gave support, and shared and received resources. “Having these bonds is so healthy. I don’t ever want anyone to feel alone like I felt at the beginning,” she says.
That’s why Filloon is now volunteering as a peer supporter for Kaiser Permanente. “I want to be there for other young women with breast cancer. I don’t want them to have to search for somebody their own age to talk to like I did,” she says.
Blogging Promotes Healing and Supports Other Young Mothers
Mama’s Got This is Filloon’s blog about her experiences with breast cancer. She started the blog to update friends and family on her breast cancer journey.
Soon, she found that writing her blog also helped her heal. “I would write these things down and let them go,” she says.
Filloon also shares her story so that other pregnant women, young mothers and other women with breast cancer won’t feel alone like she did. “I want to inspire anyone who may need it in whatever way that may be,” she says.
What Does the Evidence Say About Social Support?
“Extensive evidence shows that social support protects us from disease and death and enhances recovery from illness,” says Dr. Jonas.
The Society for Integrative Oncology says that there is strong evidence for support groups and counseling, which are often considered part of regular cancer care.
In women with breast cancer, Susan B. Komen says that social support may:
Reduce:
- Anxiety and stress
- Mood problems and depression
- Fatigue
- Pain
Improve:
- Stress
- Mood
Find Support in Your Area
You can find support services and programs near you in many ways, including through:
- Your cancer center
- The American Cancer Society
- Susan B. Komen
Most cancer centers today offer support groups and counseling along with medical care. Ask about what’s available at the cancer center where you’re being treated.
The American Cancer Society has free support programs and services to help you and your loved ones.
Susan B. Komen’s breast care helpline can help you find local, online or telephone support programs. Call 1-877 GO KOMEN (1-877-465-6636).
YOUR OPTIMAL HEALING ENVIRONMENT
Each person has an inherent healing capacity. And each of us can create our own optimal healing environment to bring out that healing capacity
4 ENVIRONMENTS FOR HEALING
Four environments work together to support health, wellbeing and healing:
- Internal
- Interpersonal
- Behavioral
- External
“Through small changes in your daily life, you can increase your body’s ability to heal.”
The Internal Environment: Mind & Spirit
Your mind, emotions, wishes and intentions make up your internal environment. Healing and a feeling of personal wholeness only occur when the mind, body and spirit are in balance.
A healing intention is a conscious determination to improve your health or the health of another person. When you have a healing intention, you:
- Expect an improvement in wellbeing
- Hope that the desired health goal can be achieved
- Understand the personal meaning attached to illness and suffering
- Believe that healing and wellbeing will occur
Personal wholeness is the feeling of wellbeing that occurs when your body, mind and spirit are in harmony and balance.
Ways to Create Your Optimal Internal Environment
Mind and body practices such as meditation support wellbeing and recovery from illness.
“Nurturing healing relationships are one of the most powerful ways to stimulate, support and maintain wellness and recovery.”
The Interpersonal Environment: Social & Emotional
Healing relationships are social and professional interactions that foster belonging, wellbeing and coherence. These relationships can be with family members, friends, doctors, pastors, neighbors, co-workers and other people.
Positive relationships are healing relationships. They are loving, kind, trusting and benefit everyone involved.
Ways to Create Your Optimal Interpersonal Environment
- Accept informal support and help from family and friends
- Join a support group(s)
- Get one-on-one counseling
- Participate in an online community for women with breast cancer
The Behavioral Environment: Behavior & Lifestyle
Healthy behaviors can enhance your wellbeing and help prevent, treat or even cure disease. Making good food choices, exercising, relaxing and avoiding unhealthy behaviors are important to lifelong health and wellness.
Collaborative team-based cancer care that focuses on the patient and her family and blends complementary and lifestyle approaches with conventional medical care is another part of the behavioral environment.
Ways to Create Your Optimal Behavioral Environment
- Eat healthy
- Get regular exercise/physical activity
- Relax and relieve stress through mind and body practices such as meditation and yoga
The External Environment
Healing spaces optimize and improve the quality of care, outcomes and experiences of patients. Things that foster wellness and recovery include:
- Architectural design in hospitals
- Color choices
- Access to nature, music, art and light
Create Your Own Healing Environment
“Optimal Healing Environments: Your Healing Journey (PDF)” explores small changes you can make in your daily life to increase your body’s ability to heal.
Ways to Create Your Optimal External Environment
Change your space at home to support your healing journey. Ways to make your home a place of healing and peace include:
- Surround yourself with nature, such as natural light, nature views or art, nature sounds and flowers.
- Decorate with meaning, including photos of family and friends, objects that are meaningful to you, and symbols of faith and personal healing. Arrange furniture to encourage conversation and interaction.
- Unclutter your home and create quiet spaces for reflection.
- Create a restful bedroom:
- Choose colors that suit your mood. Warm reds, oranges and yellows energize and stimulate. Cool blue, green and violet create feelings of peace and rest.
- Muffle stressful sounds like street noise and play music that soothes you.
- Use warm, natural, indirect lighting.
YOUR HEALING JOURNEY
Now you know that integrative breast cancer care can help you heal by:
- Relieving cancer symptoms and treatment side effects
- Minimizing anxiety, stress and depression
- Boosting your overall sense of wellbeing
“Integrative therapies can be very empowering,” says Dr. Greenlee. “They can help you take care of yourself as you’re going through treatment for breast cancer and improve your overall sense of wellness.”
TRY APPROACHES WITH STRONG EVIDENCE
Current evidence for complementary and lifestyle approaches in cancer care is strongest for:
- Mind and body practices such as meditation and yoga
- Healthy eating, especially eating a lot of vegetables and fruits
- Getting regular exercise/physical activity
These approaches will also help you stay healthy after completing your cancer treatment.
BE CAUTIOUS OF CANCER CLINICS WITHOUT GOOD EVIDENCE
Most patients with cancer will come across information about unproven, alternative cancer treatments and clinics around the world, such as treatments and clinics in Mexico, Germany and other locations. Many of these clinics will offer dozens of experimental and unproven treatments and make major claims of success.
Be cautious about these clinics, claims and treatments. Their results have rarely been validated nor have the treatments been carefully investigated. Pursuing these types of therapies in “last ditch” efforts is more likely to:
- Cost considerable money
- Reduce quality of life
- Require travel away from friends and family
- Result in a need for emergency care that may not be available
- Interfere with a good end of life
While many of these clinics are using treatments that should be further investigated, we do not recommend traveling there to receive treatment until they are proven.
WORK WITH YOUR DOCTOR AND CANCER CARE TEAM
Always use complementary and lifestyle approaches along with your conventional cancer treatment. Work with your doctor and other members of your cancer care team to choose and use complementary and lifestyle approaches. Your team knows which approaches are right for you, and which are safe and effective for people with cancer. You can use social support on your own.
While evidence about the safety and effectiveness of complementary and lifestyle approaches for cancer is growing, many questions aren’t answered yet. Experts do know that:
- Some approaches are safe and effective for people with cancer
- Some approaches can interfere with cancer treatment or don’t work. There’s not enough evidence yet to
know whether many complementary and lifestyle approaches are safe and effective.
We hope that this guide will help you heal during your breast cancer journey.
“Cancer is scary, and conventional treatments are often harsh and only partially effective,” says Dr. Jonas. “Integrative oncology—the combination of evidence-based conventional, complementary and self-care approaches—can make the experience and outcomes much better than using any one of these approaches alone.
“If you have been diagnosed with breast cancer, work diligently to put together your integrative oncology team. You and your family will be grateful you did.”
RESOURCES FOR YOUR HEALING JOURNEY
COMPLEMENTARY APPROACHES
Greenlee H, DuPont-Reyes M, Balneaves L, et al. “Clinical practice guidelines on the evidence‐based use of integrative therapies during and after breast cancer treatment,” CA: A Cancer Journal for Clinicians. April 2017.
See Table 2 for information about providers of complementary approaches.
Lyman GH, Greenlee H, Bohkle K, et al. “Integrative Therapies During and After Breast Cancer Treatment: ASCO Endorsement of the SIO Clinical Practice Guideline,” Journal of Clinical Oncology, DOI: 10.1200/JCO.2018.79.2721 Journal of Clinical Oncology 36, no. 25 (September 1 2018) 2647-2655.
National Center for Complementary and Integrative Health.
Complementary and Alternative Medicine, American Cancer Society.
NUTRITION, DIET AND PHYSICAL ACTIVITY
Heal Well: A Cancer Nutrition Guide (PDF). American Institute for Cancer Research, the LIVESTRONG Foundation, and Savor Health™ (also includes information about physical activity).
Nutrition for the Person With Cancer During Treatment, American Cancer Society.
How to cope with common eating problems, American Cancer Society.
Dietary Supplements: What Is Safe?, American Cancer Society.
Environmental Working Group:
Dirty Dozen: EWG’s 2018 Shopper’s Guide to Pesticides in Produce™
Clean Fifteen: EWG’s 2018 Shopper’s Guide to Pesticides in Produce™
Rebecca Katz, The Cancer-Fighting Kitchen, Second Edition: Nourishing, Big-Flavor Recipes for Cancer Treatment and Recovery.
Physical Activity and the Cancer Patient, American Cancer Society.
FINDING TRUSTWORTHY INFORMATION ONLINE
Don’t Believe Everything You Read on the Internet, a guide to credible Internet information, Society for Integrative Oncology.
Finding and Evaluating Online Resources, National Center for Complementary and Integrative Health.
FROM DR. WAYNE JONAS
Optimal Healing Environments: Your Healing Journey (PDF). Dr.WayneJonas.com
Wayne Jonas, MD. How Healing Works: Get Well and Stay Well Using Your Hidden Power to Heal How Healing Works, 2018.
CONTRIBUTOR LIST

Kauser Ahmed, PhD
Clinical Psychologist Director, Simms/Mann UCLA Center for Integrative Oncology Darcie Denkert Notkin Director of Psychosocial Oncology Care
Kauser Ahmed, PhD, is a clinical psychologist and the Director of the Simms/Mann UCLA Center for Integrative Oncology. She has more than 16 years of experience in caring for patients and families touched by cancer and in directing the center’s multidisciplinary psycho-oncology training program. Dr. Ahmed has played a critical role in establishing the psychosocial protocols for many of the oncology clinics at UCLA and has a particular interest in the unique needs of young women survivors of genetic cancers and their children. She was awarded the “Outstanding Clinical Care Award” by the American Psychosocial Oncology Society in February 2017.

Lynda G. Balneaves, RN, PhD
Associate Professor College of Nursing, University of Manitoba President, Society of Integrative Oncology
Dr. Balneaves has held academic positions at the University of Manitoba, the University of Toronto, and the University of British Columbia. Her research program has focused on the use of complementary and integrative therapies in the context of cancer and the development and evaluation of knowledge translation and decision support interventions for individuals living with cancer and oncology health professionals. She also conducts health policy and access research related to medical and non-medical cannabis. Currently, she is the president of the Society for Integrative Oncology and is deputy director of the Canadian Consortium for the Investigations of Cannabinoids.

Heather Greenlee, ND, PhD
Director, Integrative Medicine Service, Seattle Cancer Care Alliance Associate Member, Public Health Sciences & Clinical Research Divisions, Fred Hutchinson Cancer Research Center Associate Professor, Division of Medical Oncology, Department of Medicine, University of Washington School of Medicine, Past President, Society for Integrative Oncology
Dr. Greenlee’s clinical interests are integrative oncology, naturopathic medicine and cancer survivorship. Her research focuses on the use of lifestyle modifications and complementary and integrative medicine for cancer prevention and control. She uses observational studies and clinical trials to study what cancer survivors can do, in addition to conventional treatment, to prevent cancer recurrence, decrease side effects of treatment and improve prognosis. Her work has been funded by the National Cancer Institute, the National Center for Complementary and Integrative Health and private foundations.
Dr. Greenlee is an active member of SWOG within the National Cancer Institute’s National Cancer Clinical Trials Network and is past president of the Society for Integrative Oncology. SWOG is a global cancer research community that designs and conducts publicly funded clinical trials. Dr. Greenlee trained in epidemiology at the University of Washington and Columbia University and in naturopathic medicine at Bastyr University.

Rebecca Katz, MS
Consultant, speaker, teacher and chef
A nationally-recognized culinary translator and expert on the role of food in supporting optimal health, Katz has a Masters of Science degree in Health and Nutrition Education, and received her culinary training from New York’s Natural Gourmet Institute for Health and Culinary Arts.
As a consultant, speaker, teacher and chef, Katz works closely with physicians, nurses, and wellness professionals to include the powerful tools of flavor and nutrition in their medical arsenal.
She is the founder of the Healing Kitchens Institute, which trains health care professionals and cooks in how to translate nutritional science directly to the plate through taste and flavor, and the author of several books, including the award-winning cookbook The Cancer-Fighting Kitchen, Second Edition: Nourishing, Big-Flavor Recipes for Cancer Treatment and Recovery.

Gabriel Lopez, MD
Assistant Professor, Medical Director, Integrative Medicine Center, University of Texas MD Anderson Cancer Center, Department of Palliative, Rehabilitation and Integrative Medicine, Division of Cancer Medicine
Dr. Lopez provides integrative oncology consultations in MD Anderson Cancer Center’s Integrative Medicine Center. His research interests include patient-reported outcomes research and symptom management. Dr. Lopez received his medical degree from the Northwestern University, Feinberg School of Medicine. He completed his residency in internal medicine at The University of Texas at Houston Medical School. Following his residency, Dr. Lopez completed fellowships in palliative care and symptom control at MD Anderson and in hematology/oncology at East Carolina University’s Brody School of Medicine.
Valentina Ogaryan, PhD
Clinical Psychologist, Simms/Mann UCLA Center for Integrative Oncology
Dr. Ogaryan provides psychosocial care to patients impacted by cancer and their loved ones at Simms/Mann UCLA Center for Integrative Oncology. She works extensively with breast cancer patients, including serving as part of the
multidisciplinary medical team at the UCLA Santa Monica Breast Center and facilitating a breast cancer support group for women.
Dr. Ogaryan’s clinical training includes working with child and adult populations in various settings such as mental health treatment centers, inpatient psychiatric hospitals and medical centers. She specialized in psycho-oncology through a postdoctoral fellowship at the Simms/Mann UCLA Center for Integrative Oncology, in addition to pre-doctoral practicum training.
Laura Pole
President, Eating for a Lifetime
Pole is a health supportive gourmet chef, a registered nurse, certified Nia fitness instructor and a professional musician with more than 30 years of experience in health care, health education and entertaining people. She founded “Eating for a Lifetime” in 1997 and has been offering high-quality creative and individualized services ever since.
Nationally recognized for her creative and informative workshops and presentations on health and healing, Pole is also considered an authority in the field of health supportive cooking for people with serious illness. She co-developed and presented a workshop on Culinary Translation in Cancer Care, attended by oncology dieticians
from all over the world. She recently co-developed and coordinated an 11-day course on “Cooking for People with Illness” for the Natural Gourmet Institute in New York City.
Pole has authored two cookbooks for Smith Center for Healing and the Arts, Taking the Art of Good Eating Home and Soul Savory. She is a featured chef on the My Food My Health website. Pole serves as head chef and director of Nourishment Education Programs for the Smith Center for Healing and the Arts in Washington, DC. She is also on faculty for the nationally acclaimed Cancer Fighting Kitchen workshops.
ABOUT THE AUTHOR – DR. WAYNE JONAS
Dr. Jonas is a practicing family physician, an expert in integrative health and whole person care delivery, and a widely published scientific investigator. Dr. Jonas is president of Healing Works Foundation. Additionally, Dr. Jonas is a retired lieutenant colonel in the Medical Corps of the United States Army.
Dr. Jonas was the director of the Office of Alternative Medicine at the National Institutes of Health (NIH) from 1995-1999, and prior to that served as the Director of the Medical Research Fellowship at the Walter Reed Army Institute of Research. He is a Fellow of the American Academy of Family Physicians.
His research has appeared in peer-reviewed journals, such as the Journal of the American Medical Association, Nature Medicine, Journal of Family Practice, Annals of Internal Medicine, and The Lancet. Dr. Jonas received the 2015 Pioneer Award from the Integrative Healthcare Symposium, the 2007 America’s Top Family Doctors Award, the 2003 Pioneer Award from the American Holistic Medical Association, the 2002 Physician Recognition Award of the American Medical Association, and the 2002 Meritorious Activity Prize from the International Society of Life Information Science in Chiba, Japan.
Topics: Anxiety | Behavior & Lifestyle | Cancer | Depression | Diet | Exercise | Social Support | Stress Management
