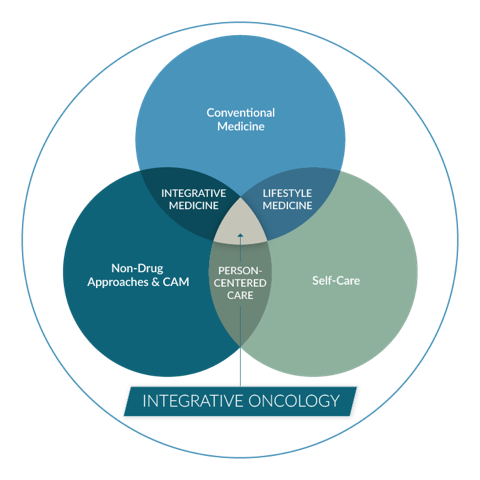
A Whole Person Approach is Integrative
Conventional treatments such as chemotherapy, radiation, or surgery are the standard of care.
But these harsh treatments can wreak havoc on the patient, causing side effects and affecting quality of life. When an individual is diagnosed with cancer, their world is turned upside down. By incorporating a whole person, integrative approach into oncology, patients will uncover ways to support and bolster their tolerance of conventional cancer care. This approach adds self-care, behavior, and lifestyle resources, as well as evidence-based complementary therapies to restore quality of life for our patients.
Whole person cancer care is a comprehensive approach that seeks to promote recovery and well-being while managing disease. The importance of what matters to the person guides treatment planning alongside what’s the matter.
As patients go through treatments, they may experience issues with sleep, pain, anxiety, financial barriers, sexual health, and many other challenges that occur outside of the exam room, infusion center, or operating theater. Inevitably, these patients look to their medical team for advice on how to manage those outer issues.
On these pages you’ll find a set of resources focused on whole person cancer care and how to incorporate this approach into your practice. Through the inclusion of evidence-based behavior and lifestyle therapies such as nutrition, movement, meditation, and others, patients will activate their individual ability to heal as they go through cancer treatment and into survivorship.
Now Available
“Healing and Cancer: A Guide to Whole Person Cancer Care” written by Alyssa McManamon, MD, and Wayne Jonas, MD published by Rodin Books, distributed by Simon and Schuster.
“Healing and Cancer” is intended to be read and actively used by teams caring for people with cancer and by caregivers and patients themselves to enhance healing, health, and wellbeing. “Healing and Cancer” directs readers to the best tools and resources available so that oncologists, primary clinicians, nurses, social workers, integrative practitioners, cancer care teams, patients with cancer and their caregivers, can incorporate whole person care into their own healing journey.
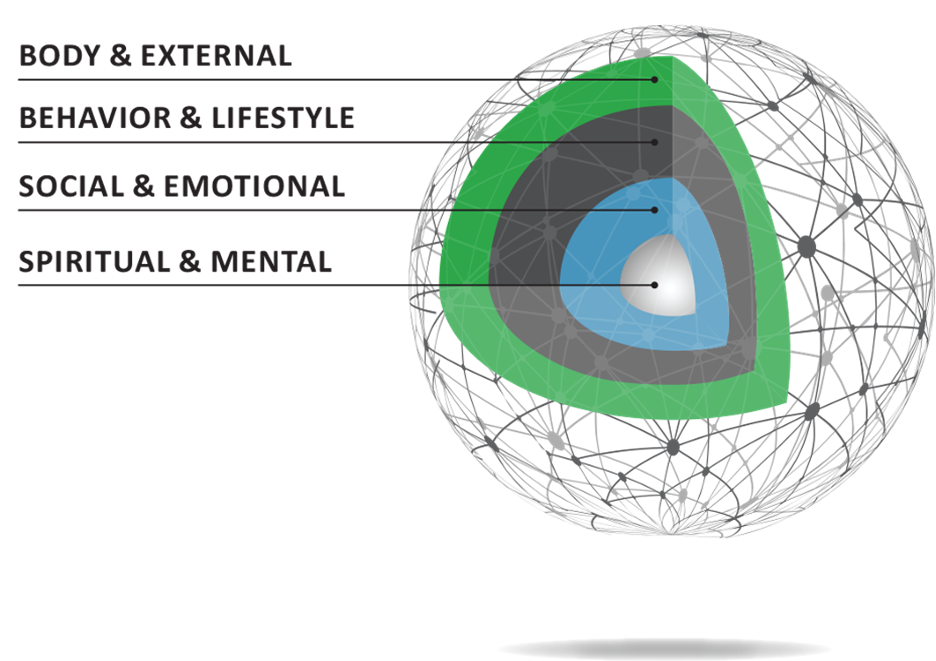
What Makes up a Whole Person
The figure illustrates the many layers that factor into a person’s ability to heal.
The outer layer represents the body and the environment. External factors influence health as much as the cellular environment.
The next layer represents the behavior and lifestyle of the individual. What is their diet made up of? How often do they exercise? What brings joy?
Social and emotional factors also have an impact on health and wellbeing. What does the patient’s support network look like? Are their emotional needs being met? Is the patient interested in talk therapy?
At the center are the spiritual and mental factors that influence the patient’s capacity to heal. By asking questions that gauge interest in connecting with a hospital chaplain or other spiritual leaders (such as someone who is trained in meditation or guided imagery), you and your team will have a better understanding of your patient and the internal and external influences on their health.

Core Reading
Whole-Person Cancer Care: A Transformative Vision for Oncology
Exploring the Roles of Patient Advocates in Integrative Oncology
Breast cancer survivorship and level of institutional involvement utilizing integrative oncology
Awareness, perceptions, and usage of whole person integrative oncology practices
Healing and Cancer by Dr. Alyssa McManamon and Dr. Wayne Jonas
Whole Person Care at Any Phase of the Journey
Whether newly diagnosed, in the middle of treatment, or in the survivorship or thrivership phase of treatment, a whole person approach to cancer is effective in empowering patients to become an equal partner in their health.
Evidence shows that patients are interested in learning more about integrative therapies, such as nutritional counseling, information about supplements, and how to manage side effects using drugless approaches.
In a survey of 1,004 patients, 60% said they strongly believe that complementary therapies are beneficial in the management of side effects and overall wellbeing.
Tools and Resources
How do we apply a whole person approach to the clinical setting?
Our guides cover the top barriers and impacts of cancer treatment, including nutrition, exercise, pain, sexual health, adolescents and young adults (AYAs) with cancer, financial toxicity, supplements, cannabis, spiritual and mental health support, and others.