Welcome to the latest essay in our “On Healing” series, where Dr. Wayne Jonas explores whole person care and the deeper dimensions of healing.
Maria sat across from me, her medical chart showing impeccable numbers—normal blood pressure, optimal cholesterol, perfect blood sugar. By conventional measures, she was the picture of health. Yet her eyes told a different story.
“I’ve done everything right,” she said quietly. “I exercise five times a week. I eat organic. I take all my supplements. But I feel empty, like something is missing.”
As we talked, Maria’s story unfolded. A successful executive, she had achieved everything society deemed valuable: wealth, status, physical fitness. But six months earlier, her closest friend had moved across the country. Her aging parents lived far away, and her work schedule left little time for community involvement or the spiritual practices that had once given her comfort.
“I don’t understand why I feel this way when nothing is physically wrong,” she said.
Maria’s situation was just one example of something I’ve observed in my decades of medical practice: health is not merely the absence of disease. Her physical needs were abundantly met, yet she suffered from profound disconnection from what matters most: meaningful relationships, purpose, and spiritual connection. By “spiritual connection,” I don’t mean organized religion but rather a sense of transcendence and finding a greater meaning in existence. This was not happening in Maria’s life, and her suffering existed in the spaces where medical tests couldn’t measure.
In the following weeks, we worked together differently. Instead of more tests or medications, we used the HOPE Note approach to explore what truly mattered to her. Maria began volunteering at a community garden, reconnected with a spiritual practice she’d abandoned, and scheduled regular video calls with her parents. Three months later, she returned with the same perfect lab values, but her eyes reflected a vitality that no medical test could quantify.
Maria’s story illustrates what research has confirmed: Human beings are complex, integrated systems. Our physical, emotional, social, and spiritual dimensions constantly interact. Here, I want to explore how understanding these interconnected aspects can transform our approach to suffering and unlock the innate capacity for healing that resides within each person, whether or not they are “sick” by conventional medical standards.
Our Human Wants and Needs
All human beings want three basic things: health (the absence of disease), wellbeing (emotional peace and a sense of social belonging), and meaning (activities that have value beyond themselves). When any of these are lacking, people suffer—through broken bodies, lack of peace, or a sense of emptiness.
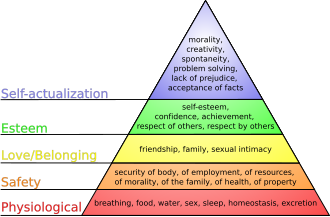
These wants are fulfilled when universal human needs are met, as described by Abraham Maslow in his classic hierarchy of human needs: physical needs (food, shelter, water, safety), psychosocial needs (love and belonging), and spiritual needs (self-actualization and self-transcendence).
When any of these needs are not met, people experience suffering in the form of a lack of wholeness, diminished capacity for healing, grief, loss of energy, and more. The needs Maslow outlined haven’t changed, but our understanding of their importance has evolved. We now recognize the profound impact of mental health and social-emotional factors on physical and spiritual wellbeing.
From Pyramid to Circle: A New Way of Looking at Our Needs
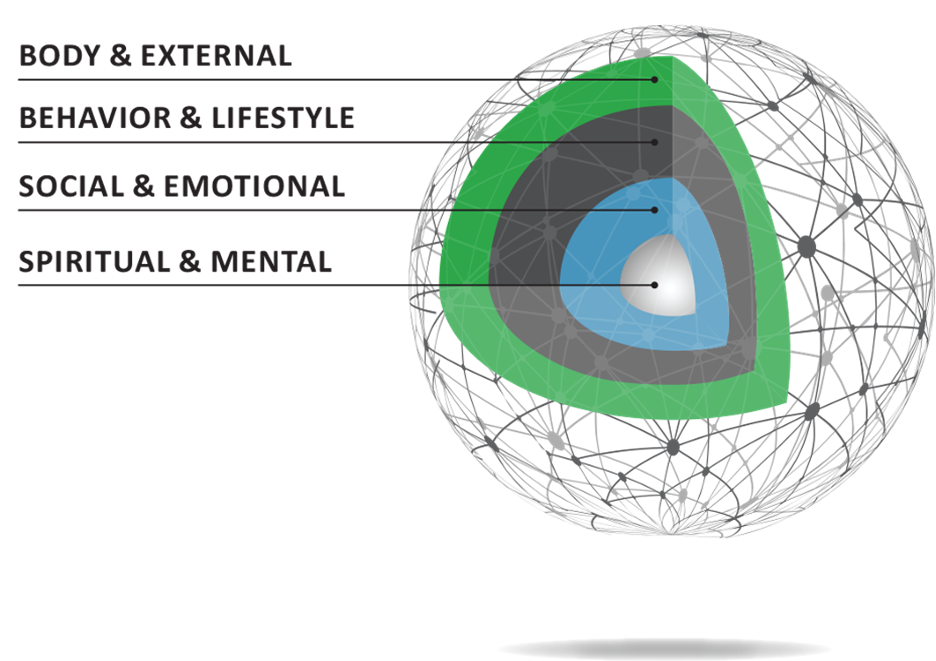
We also now know that human needs aren’t hierarchical. Those lacking basic physical needs can still find healing through rich social and spiritual connections, while those with all physical needs met may suffer from lack of meaning. Rather than a pyramid, these domains are better illustrated as a circle, with meaning and spiritual domains at the center, surrounded by social-emotional dimensions, then behaviors and lifestyle, and finally our physical body and environment.
Wholeness in Health Care
For clinicians who aspire to be healers rather than merely technicians, this holistic understanding demands that we develop tools and skills to address the whole person: body, mind, social connections, and spirit.
Consider this story from my book “How Healing Works” about a patient my daughter Maeba met during her chaplaincy residency:
A man was hospitalized with uncontrolled hypertension that resisted multiple medication regimens. When he requested a chaplain, their conversation revealed his wife had recently died—a fact his medical team hadn’t discovered. This stoic man broke down and cried for the first time. After this conversation, his blood pressure normalized, and he was discharged.
His unresolved grief manifested physiologically, resisting pharmaceutical intervention but responding to compassionate presence. What made the difference was time for meaningful conversation, attention to emotional and spiritual needs, and simply listening to connect with all dimensions of his being. Having a spiritual care provider, a chaplain, to talk with also made a difference.
What Matters
The pathway to whole person care involves asking patients what matters to them, listening deeply, and accessing resources to address emerging needs. The answer depends on two factors: the intensity of suffering and the mindset brought to that suffering.
Those without acute suffering typically focus on staying healthy, attending to body and behaviors. However, those experiencing chronic illness, mental distress, or life-threatening conditions tend to quickly access deeper existential questions. In all cases, opening a dialogue about spiritual and existential dimensions supports healing by addressing central needs. Let’s look briefly at some ways that whole person care can help relieve suffering for clinicians, patients, policymakers, and communities.
For Clinicians: The HOPE Note
Bringing meaning and spirituality into clinical practice means discussing what matters to patients, listening carefully, and following where their responses lead. This process is embodied in the HOPE Note for Whole Person Care—a simple set of tools allowing any clinician in any setting to practice whole person care.
The process begins with a personal health inventory that patients complete, helping identify underlying health drivers they most need and want to address, such as social issues, transportation problems, sleep concerns, or relationship challenges. The patient ranks these needs, guiding the discussion and placing them at the center of their care.
This approach shifts the clinical dialogue beyond physical symptoms to address the whole person. The crucial question isn’t whether we provide more care, but whether outcomes improve. The Person-Centered Primary Care Metric developed by Rebecca Etz at Virginia Commonwealth University—now validated in multiple countries and approved by the Centers for Medicare & Medicaid Services—measures the quality-of-care relationships rather than transactions. This patient-reported outcome correlates with care quality, whole person approaches, and lower costs.
Implementing this metric alongside (and eventually replacing) current measures could reduce measurement burden while improving quality and reducing costs.
For Patients: Understanding Your Own Healing Journey
As a patient, understanding that your healing involves more than just your physical symptoms can transform your health care experience. Consider completing a personal health inventory before your next appointment to identify what matters most to you across all dimensions of your being—physical, emotional, social, and spiritual.
Share these insights with your health care team, and don’t hesitate to discuss concerns beyond physical symptoms. Your social connections, sense of purpose, and spiritual wellbeing all contribute significantly to your overall health. By advocating for whole person care, you can become an active participant in your healing journey rather than a passive recipient of treatments.
For Policymakers: Three Key Changes
To implement whole person care broadly, three key policy changes are essential.
- Payment reform: We must fund management codes that give clinicians time to explore personal determinants of health and coordinate community resources. Currently, less than 5% of health care spending supports comprehensive, continuous primary care—despite evidence that this approach reduces disease burden and improves outcomes.
- Education reform: Health care teams need training in community-based care models. Costa Rica provides a compelling example, having invested in community primary care for three decades with remarkable results: decreased mortality, increased life expectancy, lower costs, and better outcomes. Even future specialists should begin with community training to see patients as whole people rather than isolated organ systems.
- Technology use: Artificial intelligence (AI) and other technologies could give clinicians more time for meaningful connection—but only if we prioritize depth over volume. When a safety-net hospital discovers that AI will free up nine minutes in a 20-minute visit, will those minutes be used for more patients or deeper healing conversations?
These changes are challenging to scale because whole person metrics are harder to quantify than traditional transactions. As health care organizations grow, competitive pressures often drive them toward fragmented care that undermines wholeness.
For Communities: Creating Healing Environments
Communities play a vital role in addressing suffering and supporting healing. Building strong social networks, creating accessible green spaces, establishing community centers, and fostering volunteer opportunities all contribute to meeting the holistic needs of community members.
When communities prioritize connection and meaning alongside physical health, they create environments where healing can flourish. This might include interfaith dialogues, community gardens, support groups, or artistic endeavors that bring people together across differences to address shared human needs.
Conclusion: The Sacred Dimension of Healing
The interconnectedness of human dimensions creates a complex system that cannot be reduced to isolated components. Sacredness—in the sense of something unique and set apart—exists in the clinician-patient relationship, within scientific inquiry, and in our acknowledgment that there are still things we don’t know. From complex systems emerge patterns and understanding that we cannot predict.
Healing involves the unique person, their social environment, physical place, and a sacred space of uncertainty. We must create room for this uncertainty by waiting and observing how elements interact. This informs both clinical practice and the systems we need—one that recognizes humans as complex ecologies whose whole exceeds the sum of their parts.
Even if we could catalog all visible aspects of human experience, we wouldn’t capture the invisible dimensions contributing to healing. Science must allow for patterns to emerge beyond our current understanding. This is the essence of complexity science. This is why healing transcends treatment—it honors both what we know and what remains mysterious in human suffering and recovery.
By acknowledging each person’s wholeness and supporting healing in all dimensions, we can transform health care from a purely transactional system to a sacred practice that truly addresses suffering in all its complexity.
References
Etz RS, Zyzanski SJ, Gonzalez MM, Reves SR, O’Neal JP, Stange KC. A new comprehensive measure of high-value aspects of primary care. The Annals of Family Medicine. 2019;17(3):221-230. doi:10.1370/afm.2393.
Healing Works Foundation. Personal Health Inventory. April 5, 2024. Accessed April 21, 2025. https://healingworksfoundation.org/resource/personal-health-inventory/.
Healing Works Foundation. The HOPE Note: A tool for adding integrative health care to a routine office visit. March 1, 2024. Accessed April 21, 2025. https://healingworksfoundation.org/resources/hope-note/.
Jonas, WB. How Healing Works: Get Well and Stay Well Using Your Hidden Power to Heal. Lorena Jones Books; 2018.
Pesec M, Ratcliffe HL, Karlage A, Hirschhorn LR, Gawande A, Bitton A. Primary health care that works: The Costa Rican experience. Health Affairs. 2017;36(3):531-538. doi:10.1377/hlthaff.2016.1319
The Physicians Foundation. New Report: U.S. primary care system crumbling amid historic disinvestment and surge in chronic diseases. February 18, 2025. Accessed April 21, 2025. https://physiciansfoundation.org/new-report-u-s-primary-care-system-crumbling-amid-historic-disinvestment-and-surge-in-chronic-diseases/.
Maslow’s hierarchy of needs. October 27, 2006. Accessed April 21, 2025. https://commons.wikimedia.org/wiki/File:Maslow’s_hierarchy_of_needs.svg.

