What is “integrative health”?
As a physician who practices integrative health, I see my patients as whole people—within families, neighborhoods and communities. They work in partnership with me to determine their unique pathways to health and wellbeing.
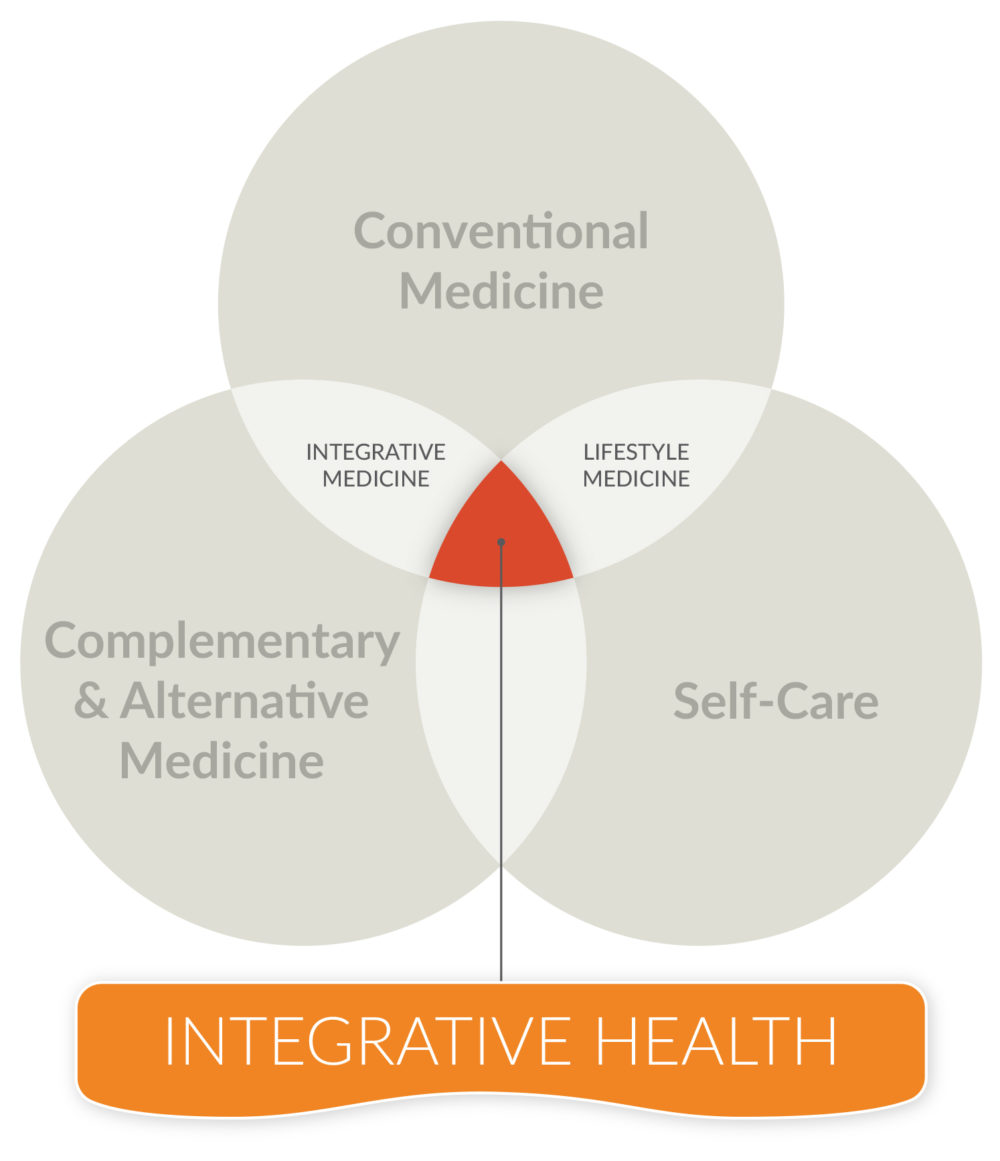
I define integrative health as the pursuit of personal health and wellbeing first and foremost, while addressing disease as needed, with the support of a health team dedicated to proven conventional, complementary and self-care approaches.
By adding self-care, the focus of health and wellness transfers from the clinician (conventional physician or complementary practitioner) to the patient. Patients become active participants in their care. This transforms the nature of the relationship between patient and care provider.
Thus, integrative health combines all three areas – conventional medicine, complementary and alternative medicine (CAM), and self-care or lifestyle medicine.
Why is this important?
We know from public health research that clinical care—whether provided by a conventional doctor or a CAM practitioner—determines only about 20 percent of a population’s health and longevity.[1] Despite this, we are bombarded by advertisements that urge us to talk to our doctors about taking the latest miracle drug or supplement.
Additionally, the United States spends more than double on healthcare than any other country in the world. And yet the World Health Organization ranks our country between 37th and 50th in terms of overall health system performance.[2] The Bloomberg Healthcare Efficiency Index has ranked the U.S. healthcare system as among the least efficient in the world.[3]
Twenty percent is a small number. If the majority of health doesn’t happen in the doctor’s office, what other factors influence our health?
It’s what happens between visits to clinicians—in our own life spaces—that has the most impact on our health.
According to research funded by the Robert Wood Johnson Foundation, the largest influences are social and economic factors, which together shape 40 percent of our health. These include factors that come from our communities and families – such as education and income – and how safe and stressful our environment is. The next largest influences are from our own behaviors, which add another 30 percent to our health and longevity.
Behaviors such as failing to get proper exercise and nutrition, and avoid smoking, alcohol and drug use, and other activities are thought to account for most of the chronic diseases in this country. These chronic diseases include chronic pain, diabetes, hypertension and cardiovascular disease.
The remaining 10 percent of health influence is determined by the physical environment – the quality of air, food and water.[4]
You mentioned that social and economic factors affect a person’s health. Do these factors also influence healthy behaviors?
They certainly do. Poverty, education, racism and other community factors have a major impact on health behaviors, the second greatest contributor to health and longevity.
Self-care and healthful practices are more difficult for those with fewer socio-economic resources. Conversely, the better the socio-economic environment, the more possible and likely it is to adopt and sustain healthy behaviors.[5]
These factors interact and influence each other. That’s why it’s critical for clinicians and patients to address these factors holistically and in partnership.
How can the health care system help patients live long and healthy lives despite the socio-economic challenges?
That is of course the key question. How to get from health care to health. How to expand outside the walls of doctors’ offices and clinics.
The answer is for our health care system to reach out into the spaces where people live their lives. Physicians, administrators and other health professionals already share with their patients the importance of healthy life choices. But the critical factor is for providers to address with patients how to implement those behaviors within their specific home situations, neighborhoods, and communities.
One way physicians can do this is by learning from patients what they need.
For example, I ask a series of questions geared to discover which aspects of each person’s life either promote healing or stand in the way of healing.[6] These questions address their body and environment, lifestyle and behavior, social and emotional factors, or mental and spiritual factors.
Together, physician and patient develop a meaningful healing plan—including trackable goals—that fit into the patient’s life.
Do you have an example of how that can be done?
One of my patients came to me with chronic, intense back pain. She was receiving physical therapy and acupuncture, but neither was helping.
We began by exploring the activities that gave her the most meaning and joy in her life. She told me that she used to enjoy yoga classes, but now she was in too much pain to go to a class. When she did go, it often injured her further.
I knew that there is good evidence that yoga is an effective treatment for back pain – if delivered properly. So, I referred her to a practitioner who was an expert in therapeutic yoga for back pain. The practitioner taught her effective (and safe) stretches for her back condition that she could do at home. Additionally, the patient learned stress reduction techniques such as meditation.
After several weeks of incorporating these techniques into her routine, the patient emailed me that she was pain-free for the first time in a decade. Guidance on using good evidence and proper provider qualifications made a difference in achieving effective self-care.
Why did this integrative health approach work for this patient?
The therapeutic yoga stretches helped stimulate her own natural healing response and reduce her pain.
This was possible because, rather than prescribe a pill or some other passive intervention, we reached into her own life to find an active and meaningful activity she could do at home – and connected that to good evidence and a qualified professional.
How does an Integrative Health approach overlap with the push for patient-centered care?
As I explained, solid evidence demonstrates that good health is determined mostly by what goes on during everyday life rather than inside the walls of medical offices and clinics. Person-centered care attempts to do this also.
Therefore, it makes sense to reach into patients’ lives to explore those factors that have the most influence on their health. These are social and emotional factors, personal behaviors, mental and spiritual factors, and the physical environment.
To me, this is the true meaning of patient-centered care. Patient-centered care is putting the patient in the driver’s seat, with the clinician providing navigational guidance from science, along with healthy doses of listening, empathy and teamwork [7].