I’ve often wondered what will be the first signs that our health care system in the U.S. is shifting toward whole person, preventative care. The first hint I got that we may be reaching this tipping point came from a comment my wife made after returning from an appointment with her dermatologist.
While sitting in the exam room waiting for the dermatologist to come in and do her regular skin cancer exam, she noticed a TV. It was not showing a news program or a game show or advertising the latest drugs or procedures for improving your complexion—it was streaming information about whole person healing.
The television in this physician’s office was sharing information about how to stay healthy and live a long, functional life—most of it having nothing to do with dermatology. The screen showed detailed information about the importance of healthy eating, exercise, stress management, and sleep for maintaining one’s health. There was even information about improving health after a diagnosis. Here was my wife, in to see the doctor about her skin, but also getting information about whole person healing.
I wrote this off as an anomaly until I had the opportunity to shadow the chief of internal medicine at the hospital where I work. He was onboarding me with the hospital’s new electronic health record (EHR). He did it by showing me how he used the new EHR during a wellness visit with a retired Navy officer. The new EHR was complex to use, but the doctor praised its flexibility for customizing templates specific to an individual’s practice. He had customized several things for his standard wellness visit.
The patient was a generally healthy 76-year-old male, although he had hypertension, pre-diabetes, and osteoarthritis, status-post two knee replacements. After reviewing his hypertension and cholesterol levels as well as their drug treatments, the doctor pulled up a template to do a diet assessment. In less than five minutes he had a snapshot of how the patient ate and made some recommendations on moving towards the low-sodium, plant-focused DASH diet to help lower his blood pressure further. The DASH diet—or Dietary Approaches to Stop Hypertension diet—is a dietary plan with the goal of heart-healthy eating.
Without prompting, the doctor then asked the patient about exercise and what he did to keep fit. Out came another template, which incorporated the guidelines from the American College of Sports Medicine on maintaining core strength and aerobic fitness in older adults. A quick discussion adjusted the patient’s exercise routine to fit those evidence-based guidelines.
Soon the doctor had ascertained from the patient (and I imagine used templates to record) stress levels and social support. No problems there.
After the visit, the doctor pointed out to me that the new EHR was not simple to use out of the box, but if one spent considerable time (in his case more than 40 hours) customizing it to one’s practice needs, it could eventually be a timesaver and allow the application of a broader number of services.
This application into the EHR created a whole person care visit.
Perhaps the chief of medicine and my wife’s dermatologist were exceptions to the norm. These examples made me curious about the data. Was health care shifting toward whole person care?
Then I had the opportunity to assist with a New England Journal of Medicine (NEJM) Catalyst survey of health care leaders to find out what they were doing and what they planned for the future in regards to whole person, integrative care.
The results of that survey stunned me. The survey comprised almost 1,000 top clinical and health care leaders from around the world as part of NEJM’s insights council. These individuals are system leaders and prominent clinicians selected to provide cutting-edge feedback on what those in health care are doing and thinking.
Here’s what they said when it comes to whole person, integrative care.
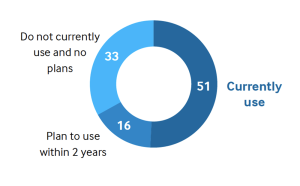
- Fifty-one percent use and 16% more plan to use integrative health care practices.
- Seventy to 80% of practices routinely incorporate exercise, nutrition, and mental health services into their systems now. Thirty to 50% already provide acupuncture, massage, meditation, and spiritual services. The majority use groups to help educate patients and deliver these services.
Use of Integrative Care at Various Organizations (Global Percentage)
In the classic 1983 book Diffusion of Innovations on how new ideas spread, Everett Rogers said that when more than 20% of the population routinely uses a particular behavior or practice, it is approaching the tipping point—the threshold for spreading throughout the culture.
Each of these examples—the tips for healthy living on the television at my wife’s dermatologist’s office, the chief of medicine’s patient-customized EHR, the data from the NEJM Catalyst survey—shows the breadth of whole person care, how it is being used in practice, and how patients are positively impacted.
Have we reached that tipping point for healing and whole person care in medicine?
I think so.
Take Your Health Into Your Own Hands
Drawing on 40 years of research and patient care, Dr. Wayne Jonas explains how 80 percent of healing occurs organically and how to activate the healing process.

