I recently had an interaction that surprised me. I was speaking with a health systems administrator who was interested in understanding the efficacy of the efforts his team was making related to delivering whole person care. He and his researcher were stuck. What should they be studying? How could they measure the impact?
In my 40 years as a researcher, advisor, and practitioner, I knew that the answers were well-established and accessible. This may sound controversial, but what we measure should be relevant and remain constant—especially when the way we practice changes.
Let me explain.
The Core Dimensions of Health Systems Performance
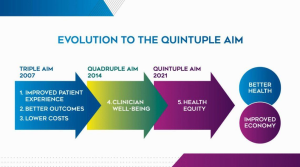
In 2007, the Institute for Healthcare Improvement developed the Triple Aim framework, which called out three dimensions to optimize a health system’s performance: patient experience of care (quality and satisfaction), population health, and costs. In 2014, with provider burnout emerging as a crisis within itself and as a barrier to delivering high-quality care, the framework was enhanced with a fourth element: improving team and clinician satisfaction. Recently, we started to recognize health equity as a fifth element in a pivotal JAMA article and was noted as the bullseye for health care measurement in an earlier article.
This “Quintuple Aim” shown below in a graphic from the American College of Cardiologists is the gold standard for measuring quality in health care.
More Tools, Same Dimensions
Measuring these five dimensions is essential no matter what approach to care we deliver. Failing to stay focused on these outcomes by using intermediary or process outcomes drives costs and burnout up and satisfaction and health outcomes down. After our discussion, I could see the light go on in the health system administrator. Not only did he now know what measures to use for his system but also which ones to eliminate.
A whole person approach to care will help us to achieve the Quintuple Aim more successfully than conventional care. As I mentioned last month, whole person care gives us more tools to achieve health, reduce costs and improve our and our patients’ experiences.
This matters not just for system administrators but for ANYONE trying to improve their practice, reduce administrative burdens, or streamline workflows. Implementing change is not easy, but it is not impossible. The Quintuple Aim is included in the new course our friends at the Center for Innovation in Family Medicine developed called Introducing Whole Person Care Into Your Practice. And measurement of whole person care ensures what we are doing is moving the needle in the right direction.
As you start to make changes in your practice or health system, I challenge you to stay focused on the core dimensions of quality health care: improved patient experience, better outcomes, lower costs, clinician wellbeing, and health equity. Staying focused on these goals will ensure that we as a nation move toward whole person care, better systems for patients, and better health for all.
Take Your Health Into Your Own Hands
Drawing on 40 years of research and patient care, Dr. Wayne Jonas explains how 80 percent of healing occurs organically and how to activate the healing process.

